- Rare diseases are life-threatening or chronically debilitating disorders that affect fewer than 1 in 2000 people.
- Approximately 80% of rare diseases are genetic in origin and symptoms can begin from early childhood to adulthood.
What are rare diseases?
Although the occurrence of each individual condition may be low, more than 2 million Australians are living with a rare disease (Australian Government, Department of Health). These diseases often involve many complex symptoms and require a range of specialised treatments.
Around 80% of rare diseases are genetic in origin and the onset of symptoms can range from early childhood to adulthood. 70% of diseases start in childhood.
The impact of a rare disease on a person’s life and their family can be devastating. Diagnosis can often take time and for many of these diseases there are no effective treatments or cures.
Over 6,000 rare diseases are characterised by a broad diversity of disorders and symptoms that vary not only from disease to disease but also from patient to patient suffering from the same disease. The fact that there are often no existing effective cures adds to the high level of pain and suffering endured by patients and their families.
Which rare diseases are we investigating at The Florey?
HCN1 gene-related epilepsy
HCN1 gene-related epilepsy is a rare genetic epilepsy that affects young children including babies who can have up to 20 seizures a day, as well as severe developmental delays.
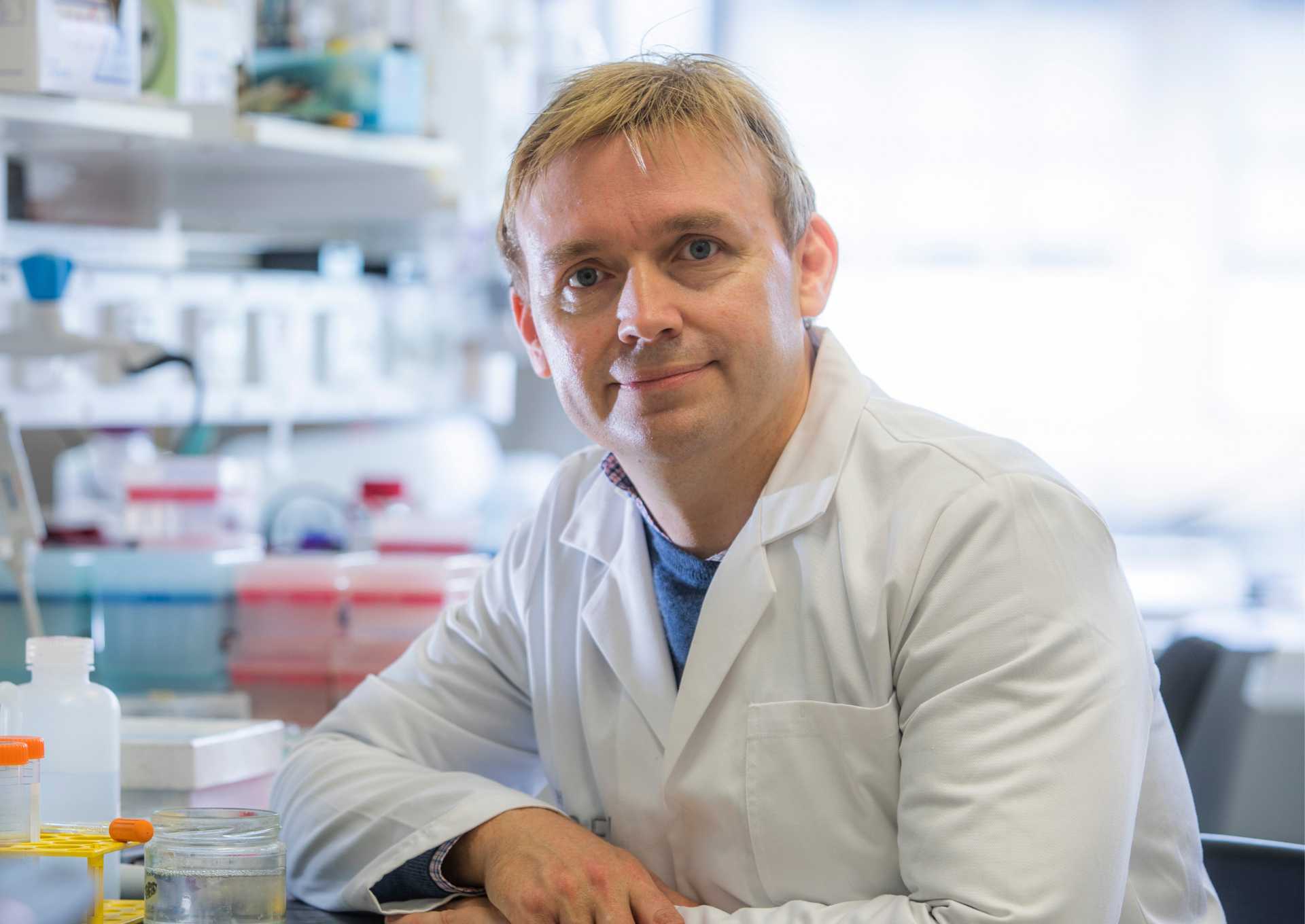
“I have seen first-hand the hope that our research can provide for patients and their families,” says Dr Lauren Bleakley.
“Gaining a better understanding of how rare genetic mutations disrupt normal brain function can lead to more informed treatment decisions being made for these patients, which can have significant positive impacts on their lives.”

Niemann-Pick Disease type C (NP-C)
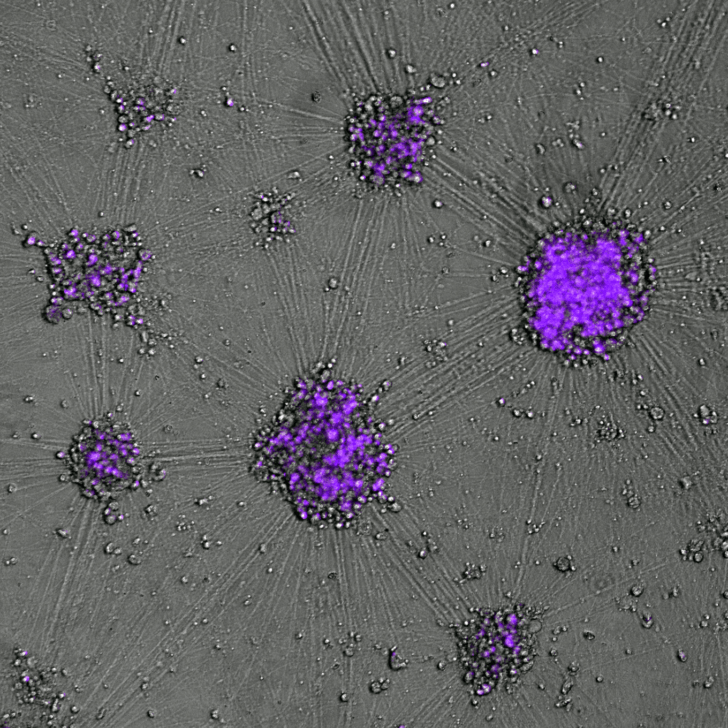
Niemann-Pick Disease type C (NP-C) is one of over 100 genetic conditions that cause childhood dementia. Due to errors in the affected gene, children born with NP-C will gradually lose their ability to think, move, and speak as they develop devastating early onset dementia.
Currently, NP-C is incurable, and half of these children will not live past their teenage years.
“My team’s research focuses on developing a new mRNA gene therapy to deliver a healthy copy of the gene to the brain, to stop the neurological damage,” says Dr Ya Hui Hung.
If we can achieve this, it will give children living with NP-C and other genetic conditions causing childhood dementia a hopeful future and allow them to live a fulfilling life.

Huntington’s disease
Huntington’s disease, neurofibromatosis and Prader–Willi syndrome include symptoms affecting brain function, cognition and behaviour and have a huge impact on affected individuals and their families. For these diseases, we have no fully effective disease–modifying therapy or cure.
“As each disease has specific genetic causes, we can model and understand each disease in great detail. It allows us to identify candidates for new therapies that we can test in our validated preclinical models,” says Professor Tony Hannan.
Our new understanding of these rare diseases will help us understand more common related conditions affecting the brain and mind, including autism, ADHD, schizophrenia, depression, anxiety disorders and dementia.
Creutzfeldt-Jakob disease
Creutzfeldt-Jakob disease (CJD) is a rare human form of one of the transmissible spongiform encephalopathies, also referred to as prion disease. Prion disease can occur as a chance event but can also be found in rare causes attributed to a genetic mutation or be acquired through a transmission event.
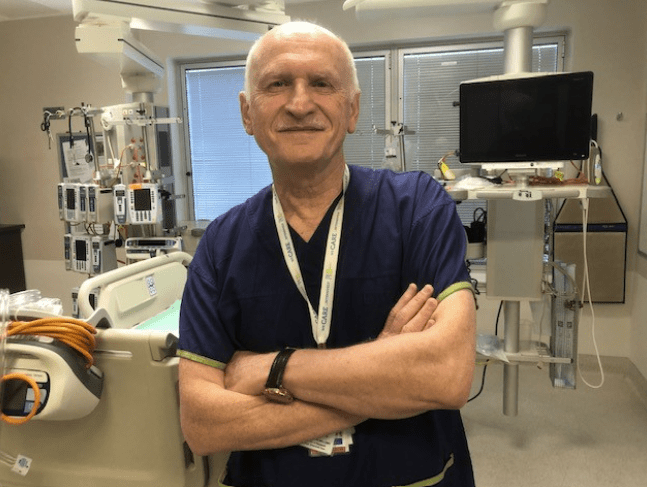
Professor Steve Collins says CJD is the most common of human prion diseases.
Although rare, prion diseases are a frequent differential diagnostic consideration in patients with subacute cognitive decline and their mechanisms of replication and transmissibility are recognised as directly relevant to much more common neurodegenerative disorders such as Alzheimer’s disease.

Multiple system atrophy
Multiple system atrophy (MSA) shares many Parkinson’s disease-like symptoms. It is a rare degenerative disease that affects movement, breathing, blood pressure and other body functions.
Around 3,000 people in Australia live with MSA. Currently there is no cure and there are very limited treatments. The average prognosis after diagnosis is currently less than 10 years.
“People with rare diseases often feel alone”, says Professor David Finkelstein.
It is important to let people know that scientists around the world are working to improve the lives of people living with MSA.
“We have been working on a compound for more than 10 years and it is now in clinical trial. It is hoped that the compound is effective in improving the lives of people with MSA. The results of the trial should be released late 2025.”

Baker-Gordon Syndrome
Named after the Florey researcher Dr Sarah Gordon, and her colleague who first identified this disease, children with Baker-Gordon syndrome can experience developmental delays, involuntary movement, poor or no speech and behavioural difficulties. This rare neurodevelopment disorder is caused by a mutation to a protein called SYTI leading to slow neural communication.
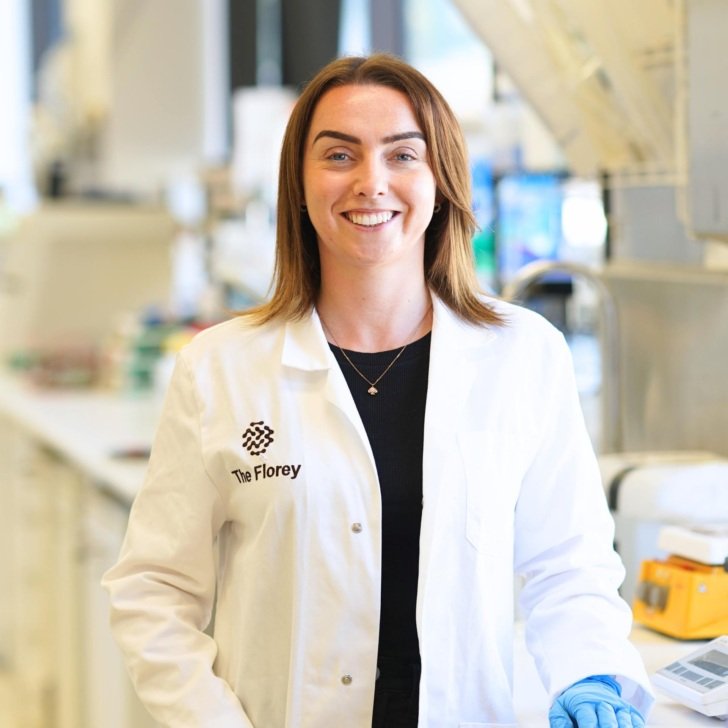
It’s been an honour and privilege to work with the families of people with Baker-Gordon Syndrome.
“There is currently no treatment or cure for this rare neurodevelopmental disorder – most children impacted by this disorder never learn to talk, and many never walk. The goal of my lab is to understand this and other rare disorders, in order to develop treatment strategies.”

Kennedy’s disease
Professor Brad Turner and his team are investigating how next-generation DNA designer drugs called antisense oligonucleotides (ASOs) could be used to target and suppress the androgen receptor gene linked to Kennedy’s disease. It is an inherited neuromuscular disorder that causes progressive muscle weakness, wasting and physical disability in men.
“Kennedy’s disease is a low-profile disease with no treatment or cure,” says Professor Turner.
Our hope is to improve the lives of people and families impacted by Kennedy’s disease.
“We are privileged to be working closely with the Kennedy’s disease community to develop a precision medicine approach, leveraging our unique patient-derived cell and models established at The Florey.”