$5.9m in funding from the Australian Government’s NHMRC Investigator Grants will support Florey research into:
- drug and diagnostic research for Alzheimer’s disease
- biomarker discovery for dementia
- understanding synucleinopathy genetics
- improving neural grafts for Parkinson’s disease.
Discovery and validation of drugs and diagnostics to propel a new era of dementia research

The emergence of new treatments for Alzheimer’s disease shows disease-modifying therapies are possible, but improvements are still needed. Current treatments focus on amyloid – a protein that is present in the brains of people with dementia – but Professor Ashley Bush said there is room to target other factors.
“My work aims to explore new biomarkers and therapies for Alzheimer’s disease through preclinical studies, imaging, and clinical trials. Over the past decade, I have built resources for these studies and will use my collaboration with the National Institutes of Health in the US to deepen our understanding of Alzheimer’s disease beyond amyloid.”
The funding will also allow Professor Bush to work on improving diagnostic tests for Alzheimer’s disease and discover new treatments.
“Previous research revealed iron elevation in the brain as a key factor in Alzheimer’s disease. I tested iron chelation therapy, but it worsened outcomes, providing a clue to the nature of the disease. My hypothesis is that iron build-up is a necessary response to protein-clumping in Alzheimer’s, leading to cell death.
“Through this funding, I will continue studying these processes using post-mortem tissue and fluid biomarkers, and will test ferroptosis inhibitors in trials,” he said.
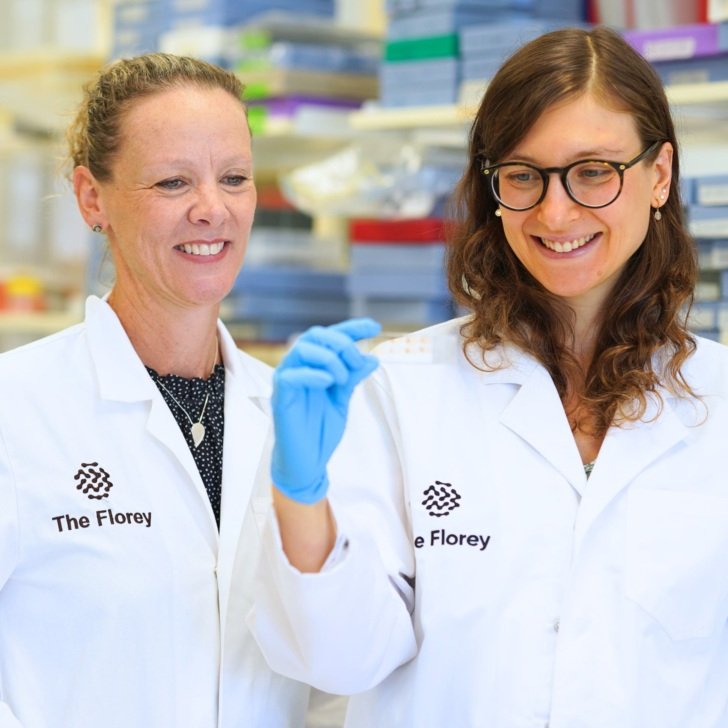
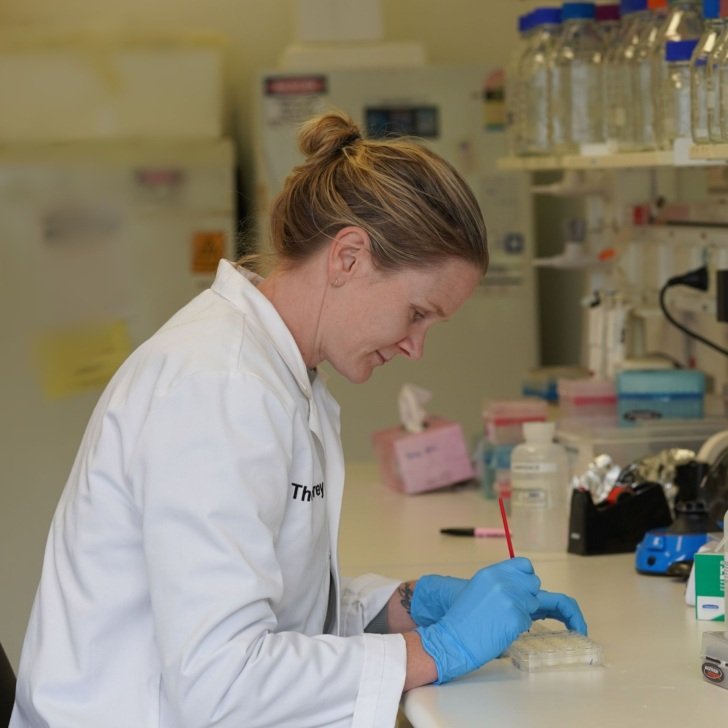
Biomarker discovery through to implementation in the new molecular era for dementia

Advancements in biomarkers have changed how dementia is diagnosed, moving from clinical opinion to biologically informed methods. Dr Pratishtha Chatterjee said these changes have been accelerated by disease-modifying therapies for Alzheimer’s disease.
“My research has contributed to demonstrating the potential of blood biomarkers for Alzheimer’s disease diagnosis, prognosis and longitudinal monitoring, and with this funding I aim to develop new biomarkers for other non-Alzheimer dementias such as dementia with Lewy bodies.”
Dr Chatterjee is also investigating cases where people exhibit Alzheimer’s disease-like symptoms but whose brains don’t show physical signs of the disease.
“My goal is to improve diagnostics for Alzheimer’s and non-Alzheimer’s dementias and understand the impact of comorbidities on biomarker levels. I will test new biomarkers in real-world settings in Australian memory clinics and refine them based on feedback from clinicians,” she said.
Decoding synucleinopathy by linking genomic variation to function

Parkinson’s disease, along with related conditions such as dementia with Lewy bodies and REM sleep behaviour disorder, are characterised by abnormal alpha-synuclein clumping in cells, Dr Carlos Gantner said.
“Genetic factors account for a significant portion of disease risk, with more than 90 genomic risk variants identified. However, their role in disease initiation, progression and prognosis are unclear. My research aims to decode these genetic risks using stem cell technology and gene editing.”
He said the project will involve creating brain organoids to model synucleinopathies, analysing gene activity to understand the role of genetic variants, and identifying potential targets for treatments to stop disease progression.
“The aim is to generate new therapeutic avenues for Parkinson’s and related disorders,” he said.
Carlos Gantner will begin his project at The Florey after he commences mid-2025.
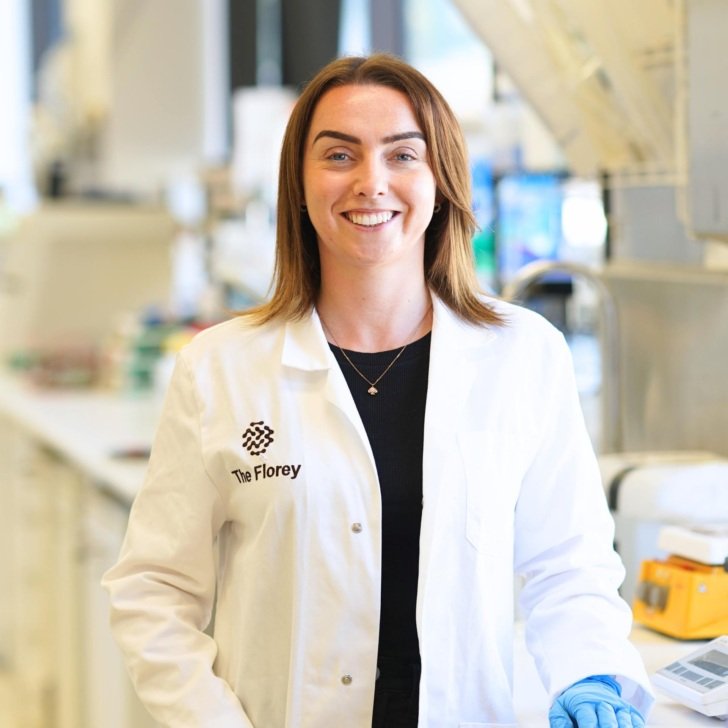
Improving the functional integration of human pluripotent stem cell-derived neural grafts

Parkinson’s disease is a neurodegenerative disorder which is predominantly known to affect movement. However, patients also experience a range of other symptoms, which current dopamine-based treatment aren’t effective at addressing.
However, Dr Niamh Moriarty said neural grafts could provide a new way of increasing efficacy of these treatments.
“My goal is to improve neural repair using human pluripotent stem cell-derived dopamine cell therapies. I will focus on new strategies to enhance the survival, integration and function of neural grafts in Parkinson’s models.”
She said the funded project will include identifying novel guidance cues to improve graft survival, using environmental enrichment to aid graft function, and assessing whether stem cell-derived grafts can address both motor and cognitive symptoms.
“These efforts will provide new insights into treating Parkinson’s symptoms and the role of cell therapies,” Dr Moriarty said.