- Florey researchers have developed an mRNA technology to target tau, a protein that clumps in the brain cells of dementia patients.
- The technique requires more research but has the potential to improve patient outcomes.
mRNA technology for Alzheimer’s disease
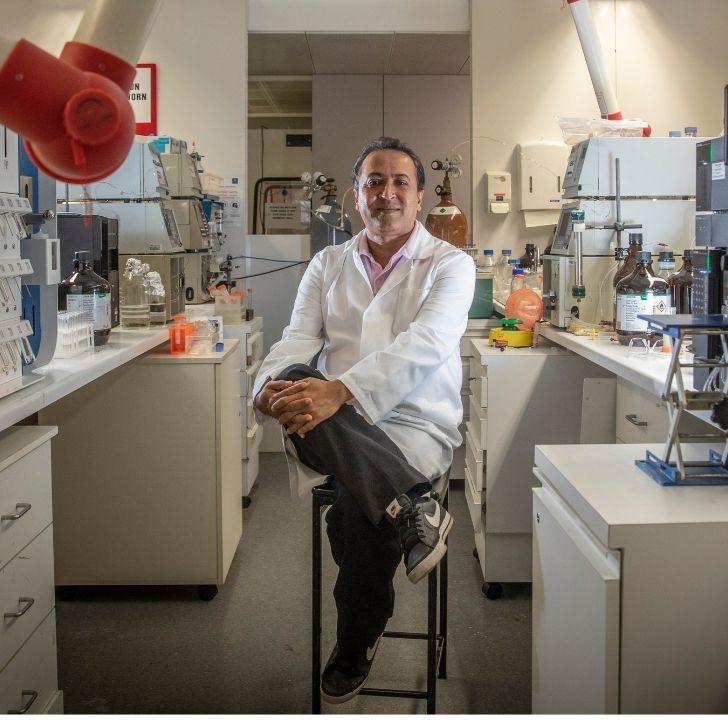
Scientists at The Florey have developed an mRNA technology approach to target the toxic protein tau, which builds up in patients with Alzheimer’s disease and other dementias.
To date, mRNA has been predominantly used for vaccines, including those used to fight COVID-19.
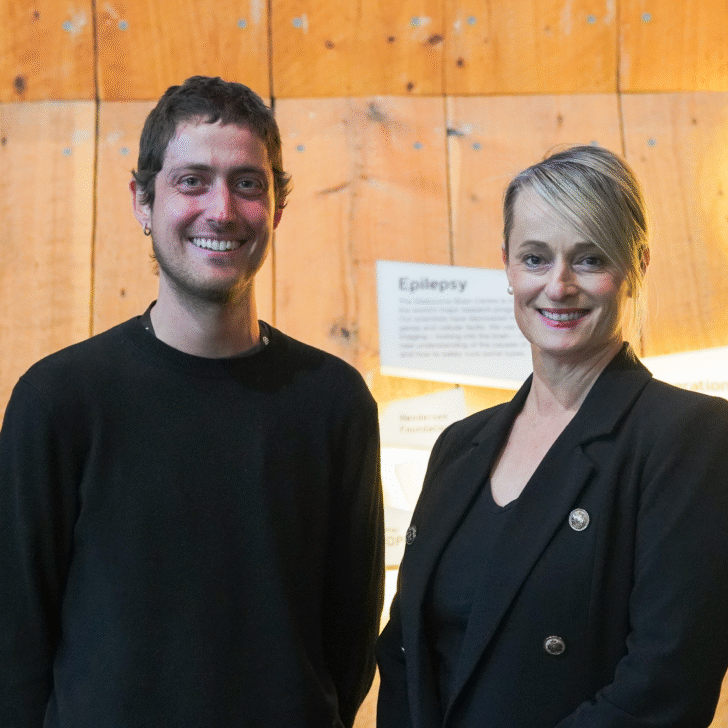
New research published today in Brain Communications establishes The Florey as a key player in the mRNA field, with Dr Rebecca Nisbet taking the technology in a new direction.
This is the first time mRNA has been explored for use in Alzheimer’s disease. Our work in cell models demonstrates that this technology can serve purposes other than vaccine development.
Dr Nisbet likened mRNA to an instruction manual for cells.
“Once delivered to the cell, the cell reads the mRNA and makes an antibody.”

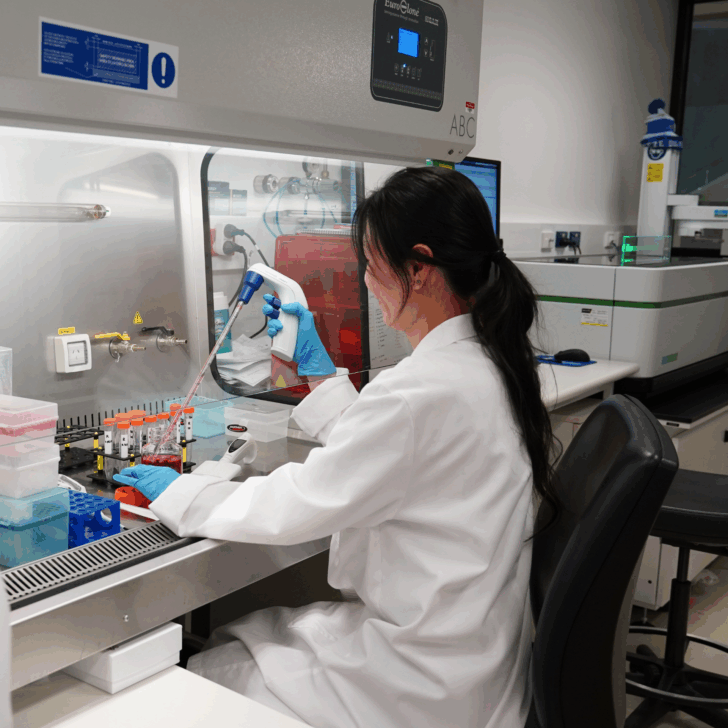
The Florey team used mRNA to instruct cells in cell models to create RNJ1, an antibody Dr Nisbet developed to target tau, a protein that clumps in the brain cells of dementia patients.
“This is the first time, to our knowledge, a tau antibody has been able to directly engage tau within the cell.”
First author on the paper, PhD student Patricia Wongsodirdjo said: “Our technique can be applied to any therapeutic antibody, and we envision that this strategy, when combined with nanoparticle packaging, will enhance targeting of toxic molecules in the brain and improve patient outcomes compared to conventional strategies.”
Dr Nisbet said RNJ1 still needed further research.
She said emerging Alzheimer’s treatments, such as lecanemab, which is approved in the USA and under consideration in Australia, are promising but expensive to make and are not an efficient way of getting an active antibody into brain cells.
“With conventional antibodies, such as lecanemab, the small amount of antibody that does enter the brain can remove some harmful plaque that lies outside our brain cells but can’t access toxic proteins such as tau, which is located in our brain cells,” Dr Nisbet said.