- A panel of researchers and health experts met to discuss how amyloid therapeutic drugs may change dementia treatment.
- Questions around amyloids include eligibility, side effects, cost, and the impact on the health and aged care workforce.
- The Minister for Health and Aged Care, the Hon Mark Butler MP, attended the event and spoke about the prevalence of dementia in Australia.
Changing dementia treatment in Australia
New treatments for Alzheimer’s disease will bring immense challenges and exciting opportunities, a gathering of leading figures in dementia has heard in Melbourne.
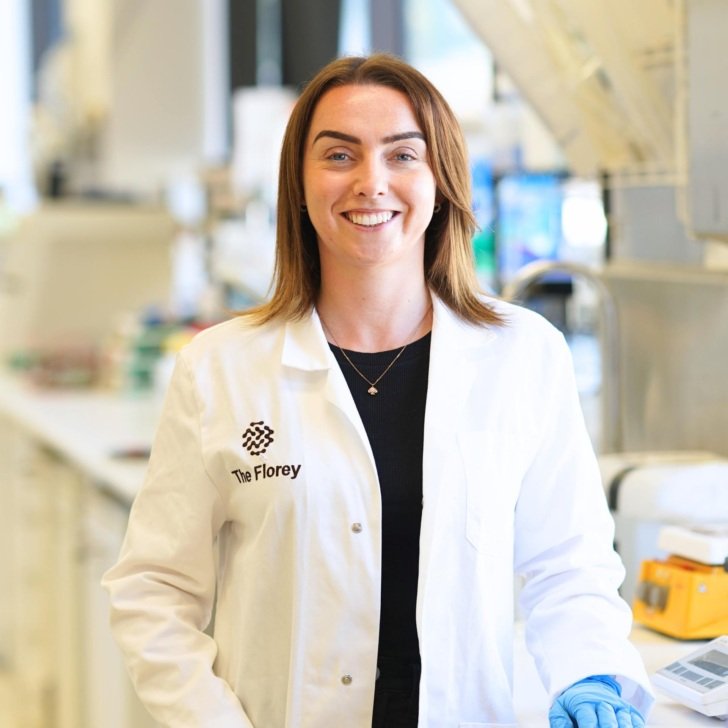
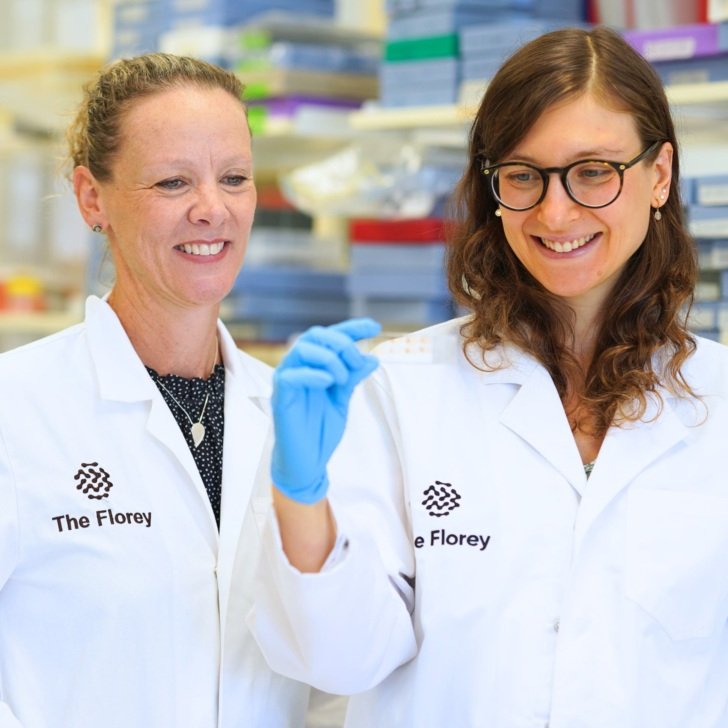
Researchers, members of the health, aged care and pharmaceutical sectors met this week at The Florey to hear how amyloid therapeutic drugs are likely to change dementia treatment in Australia.
Although the new class of drug has been proven for the first time to slow down Alzheimer’s disease in clinical trials, some questions remain around their benefits – who will be eligible, side effects, cost, infrastructure requirements, the impact on the health and aged care workforce and other challenges.
Australia’s Minister for Health and Aged Care, the Hon Mark Butler MP, spoke of how in the past 20 years, dementia’s prevalence had skyrocketed, transforming it from a fringe issue to the core business of aged care.

He said while lecanemab, the first amyloid therapeutic to be granted US FDA-approval, represented a ‘light at the end of the tunnel’, it was not a cure.
What we were dreaming of 10 years ago has the potential to become a reality. It’s not a cure, it’s a disease-modifying therapy.
Florey Director Professor Trevor Kilpatrick said now was a pivotal time for Alzheimer’s disease treatment, which is fragmented across different parts of the health and aged care system.
“This class of therapies will require an enormous shift in healthcare delivery for a large patient base. But there are huge opportunities here for both patient welfare and for acceleration of impactful research to develop even better therapies.”
There are an estimated 300,000 people in Australia with Alzheimer’s disease, but lecanemab has only shown benefit in patients in the early stages of the disease.
Professor Kilpatrick said Florey Alzheimer’s expert Professor Colin Masters had played an important role in dementia research, discovering alpha beta amyloid, the peptide that accumulates in the brain and is an essential component of Alzheimer’s disease.
“The Florey’s dementia research has gone from strength to strength since Colin’s discovery in 1985,” Professor Kilpatrick said.
Panellist Professor Scott Ayton, The Florey’s Dementia Mission Research Lead, said lecanemab is delivered by infusion every two weeks. This would be challenging for a patient population that isn’t terribly mobile.
He said it was estimated that lecanemab would cost AUD$100,000 for each Australian patient to receive an 18-month course of the treatment and have all the associated appointments and scans. “We need to factor that into the cost benefit analysis,” he said.
“There’s still a lot we don’t know (about the drug).”
Panellist Professor Chris Rowe, The Florey’s Dementia Mission Clinical Lead and Director of the Australian Dementia Network (ADNet), said he was excited that the new amyloid therapeutics are becoming available at the same time as diagnostic blood tests are being developed, which would likely support earlier diagnosis.
Professor Rowe said a rollout of lecanemab in Australia would stretch health services as patients need to have five MRI scans in the first six months as well as a PET scan to confirm diagnosis (until blood tests are available).
“The real bottleneck is going to be to see a specialist,” he said.
Professor Rowe expected the costs would come down as competitor drugs and diagnostic tests came onto the market.

Panellist Professor Amy Brodtmann, Professor of Neurology at Monash University, said the new drugs worked but had known side effects. These included a reaction to the infusion and swelling or bleeding in the brain.
“Some people, when they have these abnormalities, are only detected in (MRI) imaging, with no symptoms. Close monitoring is needed to avoid bad outcomes.”
Professor Brodtmann said the cost of the drug could lead to inequity for those unable to afford it.
“We need expectation management to explain the benefits,” she said. “The challenge is implementing this in an equitable way.”
Panellist Associate Professor Nawaf Yassi, WEHI Joint Lab Head and Deputy Director of Neurology at the Royal Melbourne Hospital, said accurate diagnosis was a crucial first step for dementia patients.
He said in the US, where lecanemab is already available, about 10 per cent of patients in memory clinics fulfilled the criteria to receive it.
“This is a new era in dementia treatment. It’s almost a new field in medical care,” he said, likening its impact to the first chemotherapy treatments for cancer.
There’s going to be a lot of work and it’s going to take time to see those improvements.
Panellist Professor Nicola Lautenschlager, Professor of Psychiatry of Old Age, University of Melbourne said it was important for all people in Australia with dementia to receive the best care available.
“I’m excited, but I think we also need to be aware that there could be a lot of families who can’t have access (to the new drugs) because their dementia is too progressed, or they have a different type of dementia.”

The Florey thanks everyone who attended: the panel; Gogglebox star Isabelle Richards for sharing her personal story of her grandmother, Emmie; ABC journalist Michael Rowland for emceeing the event; and Minister for Health and Aged Care, the Hon Mark Butler MP.