- 11 April is recognised internationally as World Parkinson’s Day.
- Parkinson’s disease is a neurodegenerative condition that affects a person’s motor function due to a loss of dopamine.
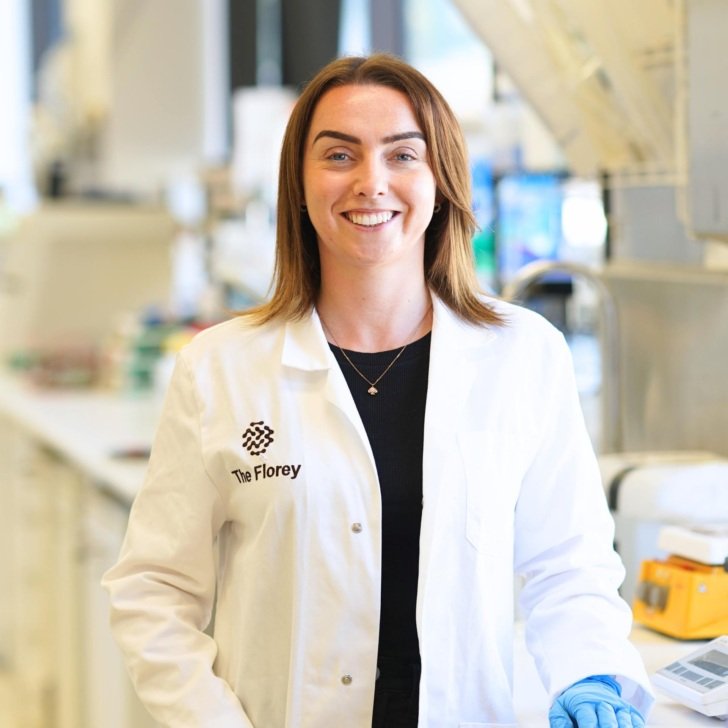
- The Florey’s Dr Niamh Moriarty is working on dopamine cell replacement strategies to restore motor and cognitive function in people who live with Parkinson’s disease.
Improving the survival and integration of neural grafts for treating Parkinson’s disease
Parkinson’s disease is a progressive neurodegenerative disorder that affects an estimated 10 million people globally and 150,000 people in Australia.
This disease causes significant impact to motor function in patients, which includes tremors, painful muscle contractions and other impairments.
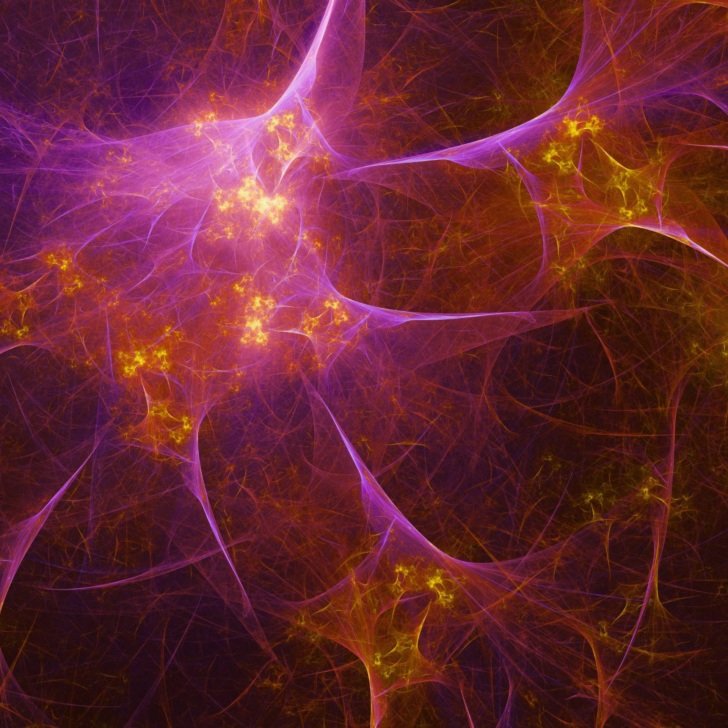
The motor dysfunction seen in Parkinson’s disease is caused by the loss of a single cell type in the brain, called the dopamine neuron.
These dopaminergic neurons normally produce dopamine, which is necessary for controlling movement, so when these cells die, you lose control over your motor function.

Current drug treatments focus on the replacement of dopamine in the brain. While they do provide significant benefit to patients, their long-term use is hindered by a loss of efficacy – their benefits do not last over time because as the disease gets worse, the replacement of dopamine is no longer enough to compensate.
Cell replacement therapies for Parkinson’s disease
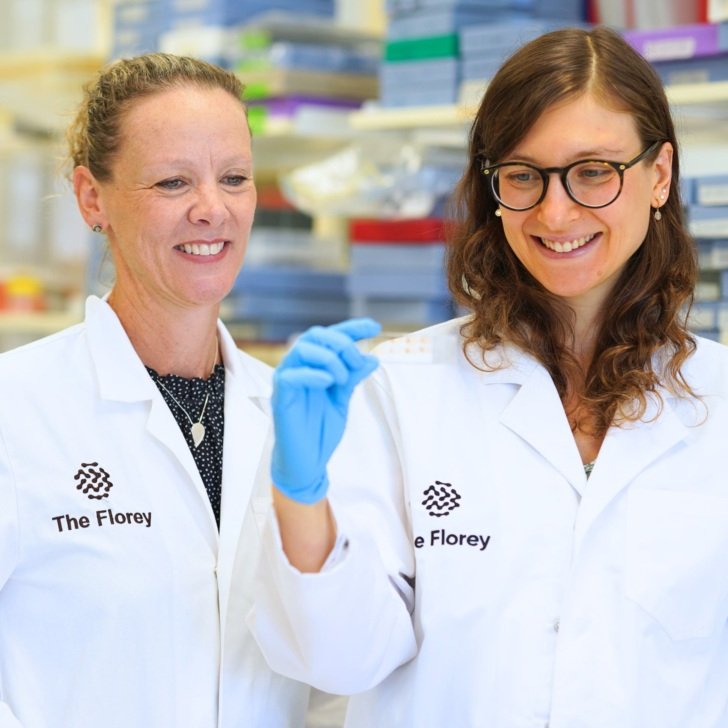
Here at The Florey, we are focused on developing and improving cell replacement strategies for Parkinson’s disease.
Cell replacement therapy involves generating new and healthy dopamine neurons, which are then transplanted into the brains of Parkinson’s disease patients (a process known as neural grafting) to replace the neurons that were lost to the disease.
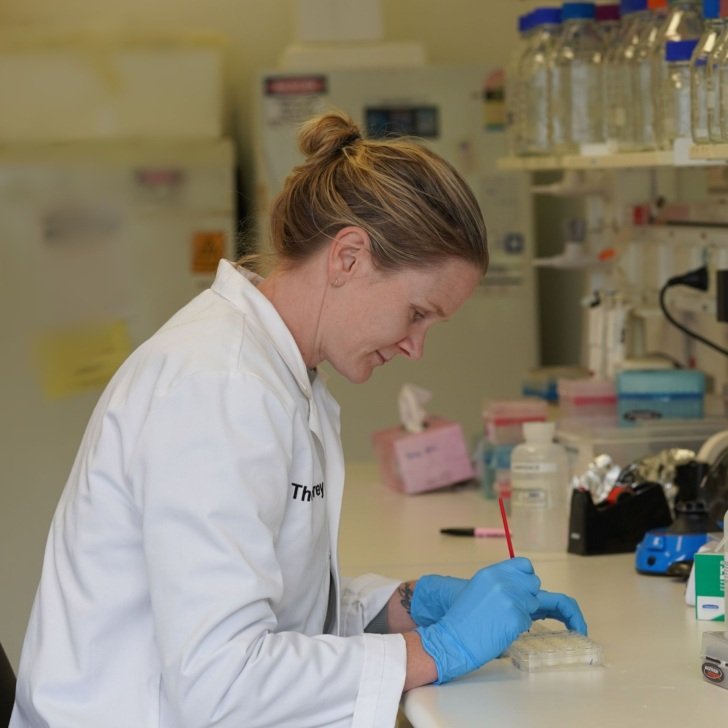
We generate these healthy dopamine neurons from stem cells.
I like to think of stem cells as your early, primitive cell. They have all the potential in the world and haven’t decided what they want to be when they grow up yet.
They can become one of over 200 cell types. So, by using very defined protocols, we can instruct these stem cells to become dopamine neurons.
Developing the next generation of dopamine cell replacement therapies
Current dopamine cell replacement strategies have shown to improve motor function by restoring dopamine activity in the Parkinson’s disease brain. However, we see poor survival and connectivity of these neural grafts within the brain, which could lead to subpar outcomes and incomplete motor recovery for patients in current clinical trials.
Our current research aims to improve the outcomes of stem cell-based therapies for Parkinson’s disease, by improving the survival of dopamine neurons after transplantation, and improving their ability to connect with the brain, which all lead to better motor recovery. We look at combined treatments and various strategies to improve the survival and integration of these neural grafts within the brain.
What’s most exciting to me about this research is its potential. I think we are only beginning to tap into the potential of stem cell replacement therapies for Parkinson’s disease.
With these new advancements and new avenues, we could develop new dopamine cell replacement therapies that could give a much more complete and well-rounded solution for patients that could cover, hopefully not just their motor, but also non-motor symptoms.

Addressing non-motor symptoms of Parkinson’s disease
When people think of Parkinson’s disease, they think of a motor disorder. The non-motor symptoms, such as impaired cognition, are just not talked about as much and may be less understood, even though they are in no way less significant.
Some of these cognitive symptoms include changes to thinking, information processing and memory.
There is an urgent need for therapies that address both motor and non-motor symptoms in this disease.
In our recent work where we have looked at dopamine cell replacement therapies for motor function, we’ve also revealed that these neurons, once transplanted into the brain, can also connect with brain regions that are involved in those cognitive symptoms of Parkinson’s disease.
Our hope for the future of Parkinson’s disease treatment is to develop hopefully a one-off treatment that targets both motor and non-motor symptoms, which would then give Parkinson’s disease patients a more comprehensive recovery from their symptoms.