- A third of patients who undergo cardiac surgery requiring the use of a heart-lung machine experience acute kidney injury (AKI), with 6 per cent needing dialysis.
- Even mild or short episodes of AKI can transition into chronic kidney disease that substantially diminish quality of life.
- During cardiac surgery, the heart-lung machine temporarily takes over the job of the heart and the lungs allowing the heart surgeons to operate.
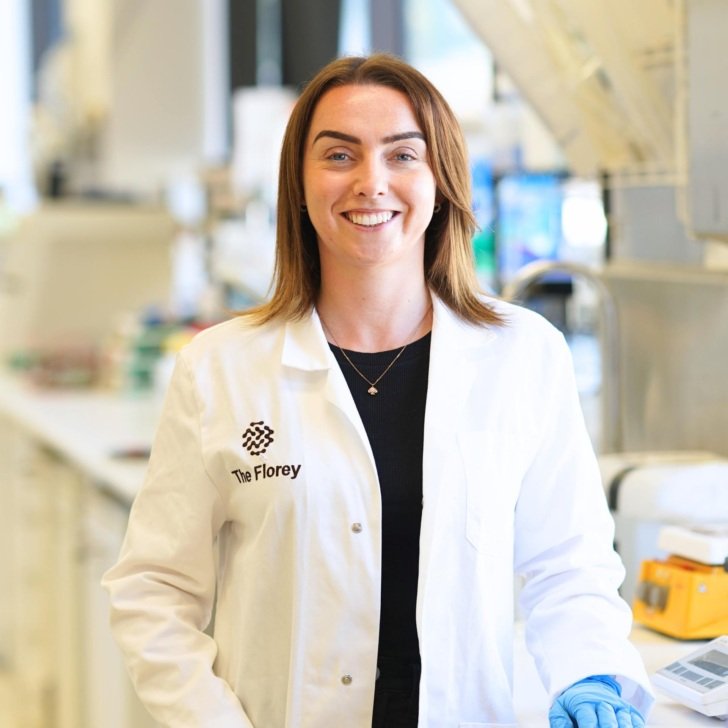
- Florey researchers are working to better understand, diagnose and treat AKI following cardiac surgery.
Cardiac surgery using the heart-lung machine harms the kidneys for longer than thought
Florey researchers in collaboration with practicing clinicians who routinely care for heart surgery patients have developed a world-first animal model to understand how cardiac surgery requiring the use of a heart-lung machine causes injury to the kidneys.
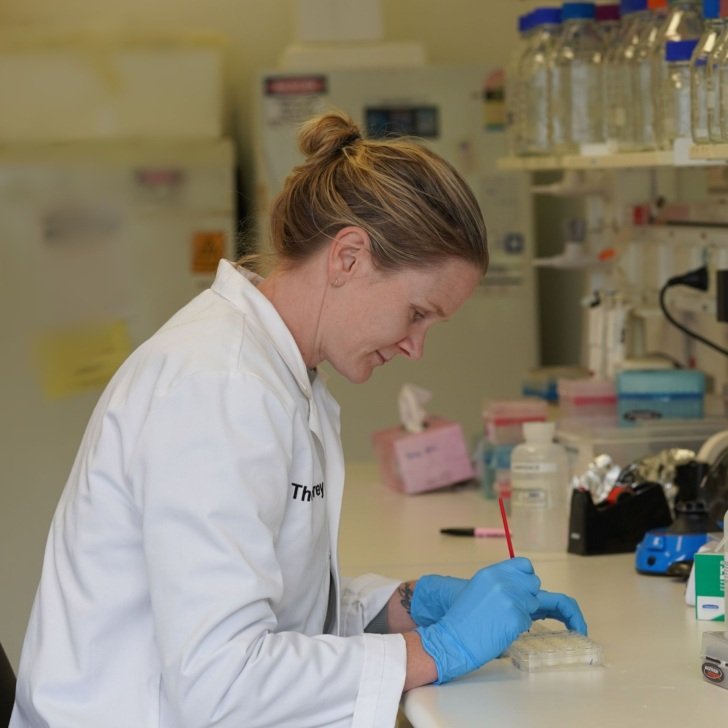
By continuously monitoring kidney health of sheep before, during and after heart surgery, Florey researchers have discovered that the surgical procedure deprives the kidneys of oxygen causing tissue inflammation, cell death and scarring.

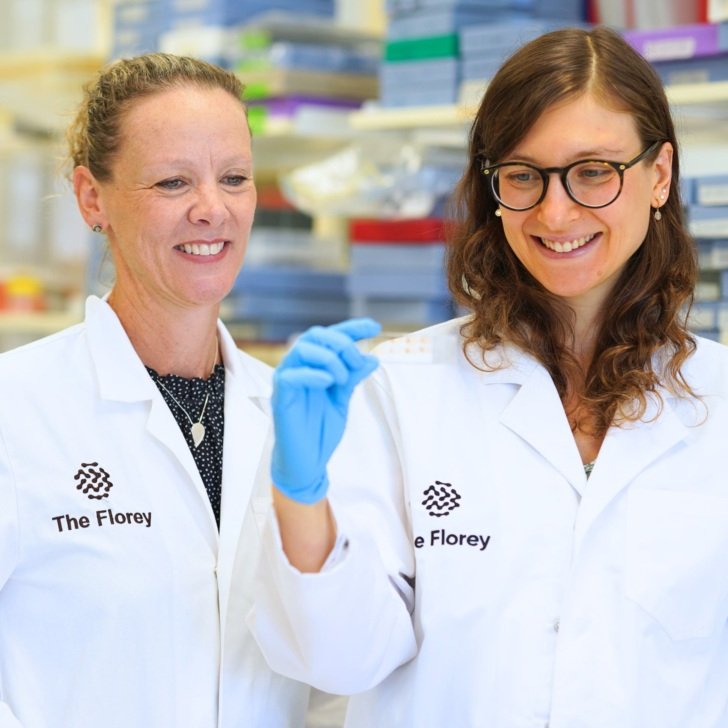
Lead researcher, Professor Yugeesh Lankadeva, Head of The Florey’s Critical Care Priority Research Area, said his team’s study, published in Anesthesiology, the peer-reviewed journal of the American Society of Anesthesiologists (ASA), provides new insights into a complex unresolved clinical problem.
“We provide robust evidence that cardiac surgery deprives the kidneys of oxygen during and well after the operation. We found that oxygen deprivation persisted over 4 weeks after cardiac surgery and was associated with inflammation, cell death and scarring in kidney tissue. This signals a link between AKI transitioning into chronic kidney disease in patients who have had cardiac surgery.”
Professor Lankadeva said the team studied 12 sheep that underwent cardiac surgery, finding:
- Blood flow and oxygen delivery to the kidneys decreased significantly when the heart-lung machine was used during cardiac surgery.
- In the first 48 hours after the surgical procedure, there was a continuing significant decrease in tissue oxygenation, with AKI occurring in 42 per cent of the animals.
- At 4 weeks after cardiac surgery, their tissue oxygenation remained significantly lower than before, while their kidney tissue had significantly more inflammation, cell death and scarring.
“This work has significantly advanced our understanding of what happens in the kidneys before, during and after cardiac surgery. Thanks to a collaborative effort between Florey scientists and practicing clinicians (cardiac anaesthetists, cardiac surgeons, clinical perfusionists, intensive care physicians) from Austin Health, Monash Health and Townsville Hospital, we have developed a clinically relevant testbed that can be used to develop mechanism guided diagnostics and therapies to reduce the development of AKI,” Professor Lankadeva said.

The paper’s first author, Dr Taku Furukawa who is a clinician undertaking a PhD at The Florey, believes that this research can improve the lives and health of countless people requiring cardiac surgery.
As a dual-trained anaesthesiologist and intensive care physician, I have seen thousands of patients suffer from AKI after undergoing cardiac surgery.
“This study provides pivotal knowledge about how this injury occurs to the kidneys during and after cardiac surgery, which lays the foundation to develop mechanism-guided diagnostics and therapies,” Dr Furukawa said.
“I really look forward to bringing these findings back to clinical practice to improve health outcomes in patients undergoing cardiac surgery after completing my PhD at the Florey.”