- Florey researchers have engineered a neural graft that flies under the immune system’s radar and evades rejection.
- Neural grafts are a realistic future treatment for many neurological disorders and for Parkinson’s disease patients this is coming close to reality, with at least 3 major clinical trials in progress.
- The technology is the next generation in neurological treatment but could have applications for a range of other kinds of transplants.
Cloaked human neural grafts evade immune detection
Florey researchers have engineered a way to fool the immune system into accepting neural grafts as part of the body, rather than attacking them as foreign objects.
The research, published today in Cell Stem Cell, could signal an end to the reliance on drugs necessary to prevent graft rejection, not just for Parkinson’s disease neural grafts, but for other cell transplants.
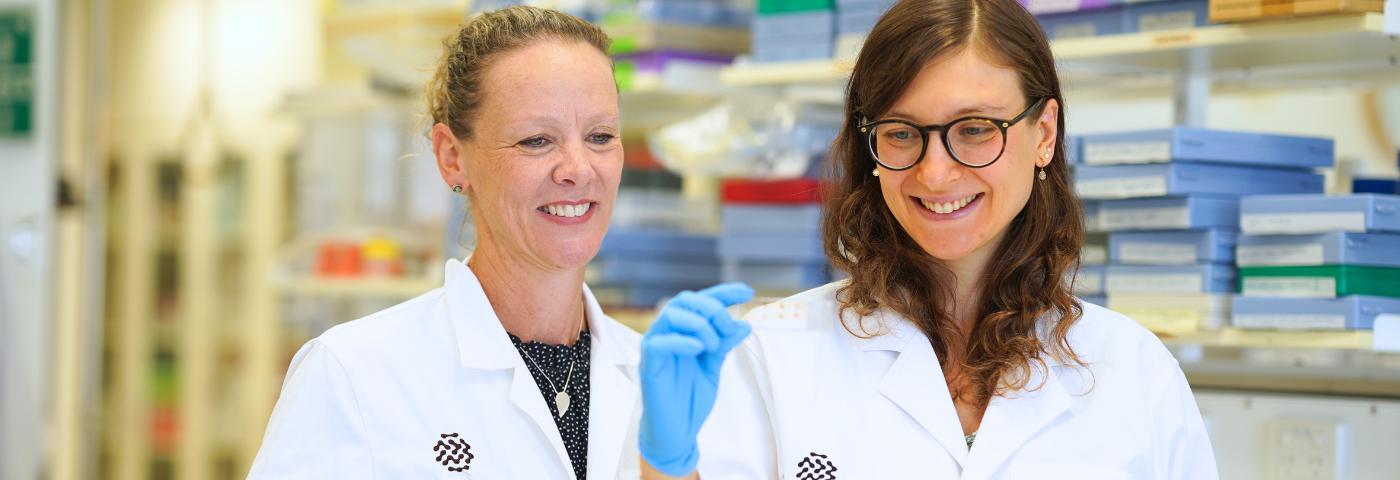
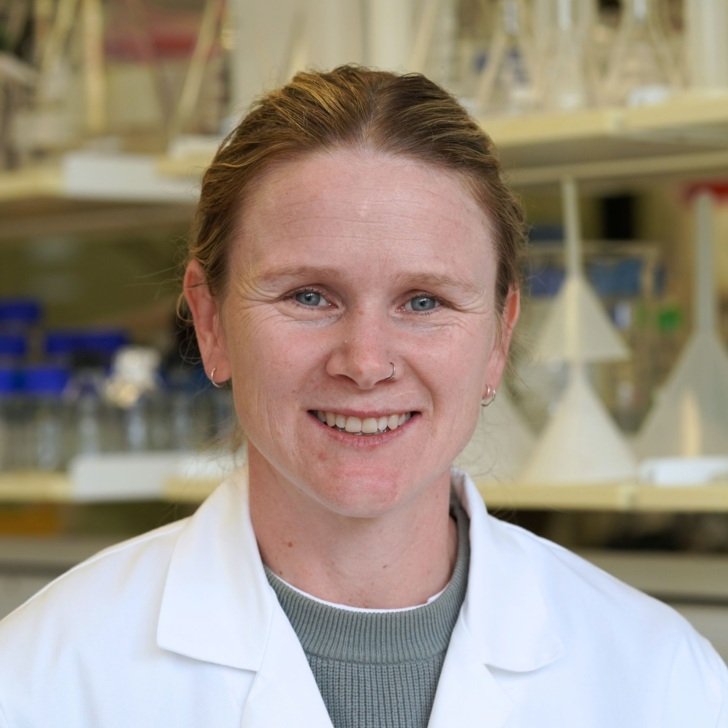
The study’s lead author, Florey Deputy Director Professor Clare Parish, Head of Stem Cells and Neural Development, said Parkinson’s disease is a neurodegenerative condition that affects an estimated 10 million people globally and 150,000 people in Australia.*
“Parkinson’s disease causes specific nerve cells – neurons – to die, leading to symptoms that include difficulties moving, tremor, stiffness, and impaired balance. Neural grafting is an emerging treatment to replace those dead neurons,” Professor Parish said.
“Human neural graft trials are underway overseas but, as with other types of organ or cell transplants, patients need to stop their body rejecting the graft by taking immunosuppressant drugs several times a day. Unfortunately, these drugs carry their own risks and side-effects.”
Professor Parish said the team, in collaboration with the University of Toronto, has taken neural grafts to the next generation, and the work could benefit other cell transplants.
We’ve engineered neurons which are like those currently in clinical trials for Parkinson’s disease, but we’ve also given them an invisibility cloak. They can hide in plain sight from the immune system. This could mean an end to the need for anti-rejection drugs.
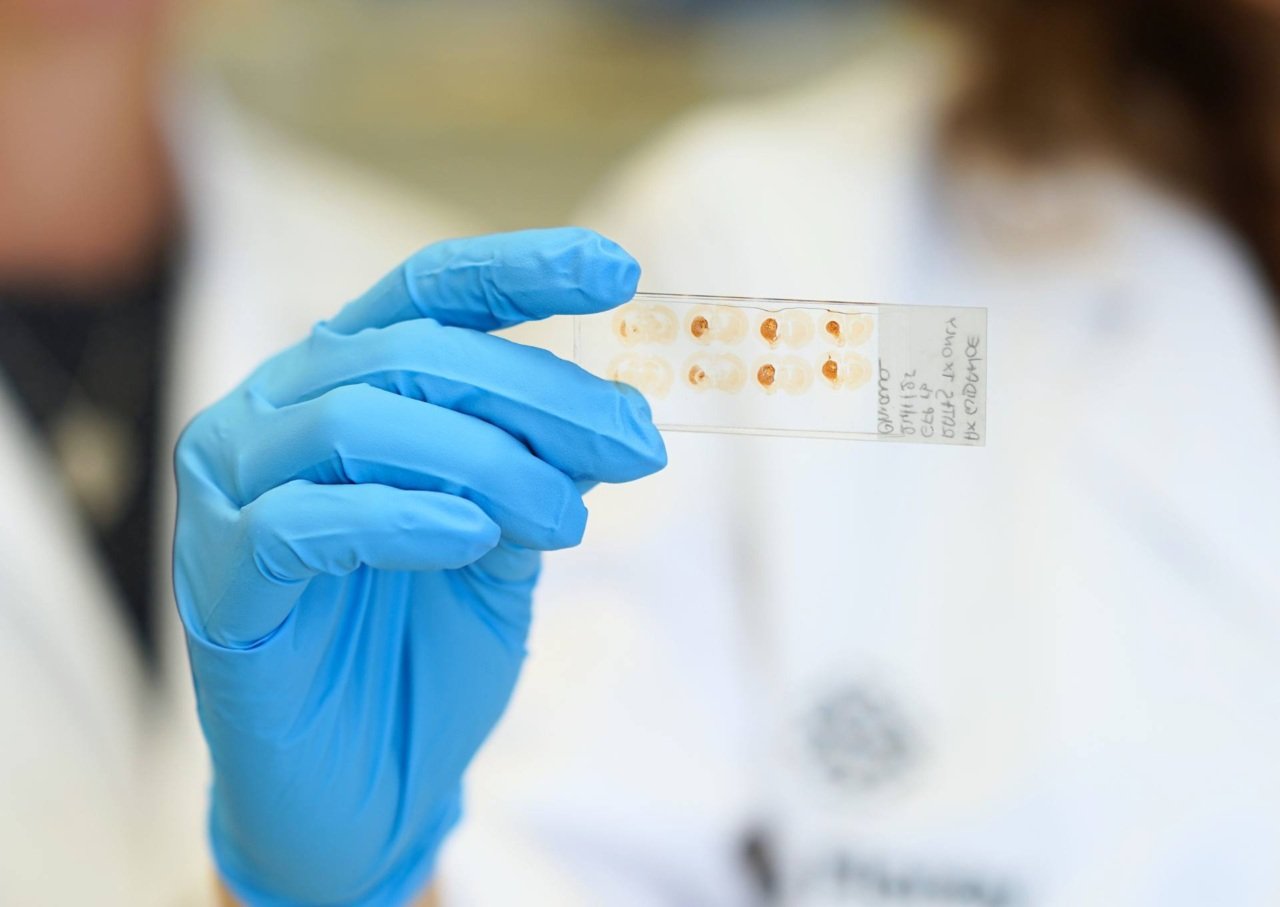
The paper’s co-lead author, Dr Chiara Pavan, who specialises in neuroimmunology, said the team tested the engineered neuronal grafts in mice with a ‘humanised’ immune system, and in rats modelling Parkinson’s disease.
“Current medications treat the symptoms of Parkinson’s disease, but these grafts target the cause by replacing dead neurons,” she said.
“After receiving their neuronal graft, the mice showed no negative effects – which is a good indication that the human immune system will accept the neurons. In rats, the symptoms of Parkinson’s disease were abolished, indicating the cloaked neurons don’t lose their effectiveness against the disease.”
Dr Pavan said the neurons also had an ‘off’ switch so that they can be activated if desired, to eliminate the risk of tumours developing from grafts.

Professor Parish said it is an exciting result and the technology has huge potential.
“We’ve made a cell product that in future could be implanted in people with Parkinson’s disease, reducing the need for anti-rejection drugs,” Professor Parish says.
Stem cells can be turned into any kind of cell, and we’ve effectively made them invisible to the immune system.
“This is the next generation of neurological treatment, and it could be used as a safe, off-the-shelf cell product suitable for treating diseases for which cell-based therapies are a viable option, such as stroke, Huntington’s disease, heart diseases and diabetes.”