- This year’s World Mental Health Day theme is ‘Mental health at work’, acknowledging that mental health and work are closely linked.
- Creating more inclusive mental health care approaches in workplaces is key for breaking down stigma and better supporting people.
We spoke to Associate Professor Jess Nithianantharajah, Head of The Florey Department of Neuroscience and Mental Health and the Synapse Biology and Cognition Group. about recognising mental health conditions in the context of work and the need for a holistic model of mental health care.
Q: Can you explain your role and your work at The Florey?
I lead a research group that’s working to understand the changes in the brain that underlie complex mental health conditions like schizophrenia and depression.
Specifically, we’re interested in knowing more about the cognitive symptoms in these conditions – which impacts the capacity to think, plan, concentrate, remember, and make decisions – and how we develop new treatments to address them.
As it currently stands, there are no effective treatments that address those symptoms, yet these can significantly impact an individual’s daily functioning, connection with society and quality of life. So we see these challenges as one of the key barriers to address.
Q: What is the importance of us recognising mental health conditions in the context of work, and in society in general?
A great outcome of World Mental Health Day is it has helped shift stigma and progress in mental health and ill-health, but there are still barriers we need to break down in society. There’s a huge spectrum of what mental ill-health looks like for different individuals, from mild to chronic.
A key for how we can better address mental health in the workplace is to develop more inclusive approaches to support and provide work opportunities for people at every level of the mental-ill health spectrum.
This engagement is critical for how well people are able to live and integrate into society, which is critical for an individual’s recovery.
At The Florey, we are working to understand the root causes of complex mental health conditions.
This understanding is important for informing prevention and early intervention – how we better identify people who might be at higher risk, for example.
In addition, understanding the neurobiological processes in complex mental health conditions is essential to drive the development of new and better therapies, which is critical for helping those chronically living with these conditions.
Q: What have you found in your research and from working with people with lived experience of complex mental health conditions?
A key point that resonates for many individuals with lived experience, carers and families is that not everyone living with the same mental health condition has the same challenges. That’s a core component of The Florey’s approach too.
Advancement in mental health care is about developing a better range of targeted, personalised therapies for people with complex mental health conditions.
Strategies such as lifestyle changes including diet, exercise, and other healthy habits can help manage some people’s symptoms. But for others, there will be a need for additional support and different pharmacotherapies.

Q: Is mental health care moving towards a holistic approach?
Absolutely. A key is to be able to provide multiple options, or a suite of therapeutic options – both pharmacotherapies and psychosocial support services are needed. One size very much doesn’t fit all to support people’s recovery.
We need to move towards having a more holistic model where it isn’t just about providing a single form of support.
It’s also about armouring carers, families and communities with the required support to wrap around people living with mental health conditions to collectively be their primary support.
So if you think about it, mental health care is a collective effort.
Q: What do you think is the role of neuroscience in creating this more inclusive society?
One of the key things that neuroscience has shed light on is that not everyone with a given diagnosis of one mental health condition looks the same.
One key learning that neuroscience has been pivotal in shedding light on is that not everyone with a given diagnosis of one mental health condition is the same.
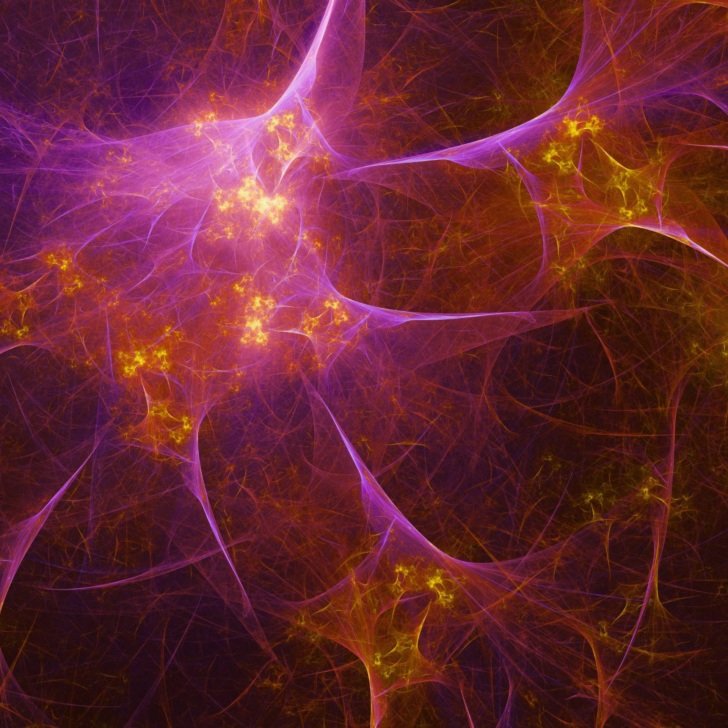
Neuroscience has revealed how the underlying neurobiology of mental health conditions is quite diverse and complex. In the brain, there are multiple processes and systems that can shift and change in a single mental health condition.
This highlights why we see such diversity in the symptoms and challenges that different people diagnosed with the same condition face, but also real challenges in developing better treatments as it’s not just about targeting one process or system to address this.
Advancing our knowledge and understanding of the biology of mental health conditions is critical for shifting the stigma on what it really means to have a mental health condition.
Stigma is often perpetuated with a fear of the unknown and a lack of understanding.
Sometimes, mental health conditions can be seen as being very subjective, as if it’s a person’s choice to behave in a certain way or experience the challenges they face. People may even question whether someone really has a mental health condition or not.
But neuroscience is providing the biological evidence of the underlying changes in the brain to inform why somebody might develop a complex mental health condition.
This knowledge contributes to developing refined objective measures of mental health conditions.
This will also have a big impact in informing treatment choice and how we better track symptom progression.