- New disease-modifying drugs to treat Alzheimer’s disease are potential game-changers and we want to help with the rollout of those medicines to improve clinical care and research.
- The Florey is on the cusp of improving the lives of children with severe forms of epilepsy.
- A new drug for schizophrenia, drug called KarXT, is on the threshold of receiving US Food and Drug Administration approval.
- Florey researchers aim to transplant neurons derived from stem cells to treat Parkinson’s disease.
A wicked problem – what’s that?
By Felicity Lewis, Explainer Editor at The Age and The Sydney Morning Herald
The term “wicked problem” was coined in 1973 in California by two professors of design and urban planning, Horst Rittel and Melvin Webber.
“Planning problems are inherently wicked,” they wrote, as in tricky rather than evil. Innovations such as drainage, sewerage, roads and water piped to homes in cities had been “truly phenomenal” accomplishments in the previous century, they said, and yet societal issues such as crime and poverty remained stubbornly resistant to one-fix solutions.
“Social problems are never solved,” they wrote. “At best, they are only re-solved – over and over again.” Space junk, climate change and the equitable provision of optimal aged care are just a handful of the issues facing humanity that have since been described as wicked problems. Professor Trevor Kilpatrick would like to add a few more – but he and his colleagues are looking for solutions all the same.
Trevor, pictured below, is a neurologist who’s expert in diseases that damage nerve fibres, especially multiple sclerosis, or MS. When not treating patients, he leads teams of researchers from various fields – biologists, geneticists and so on – who work out things such as which genes make people susceptible to MS. But that’s not all.

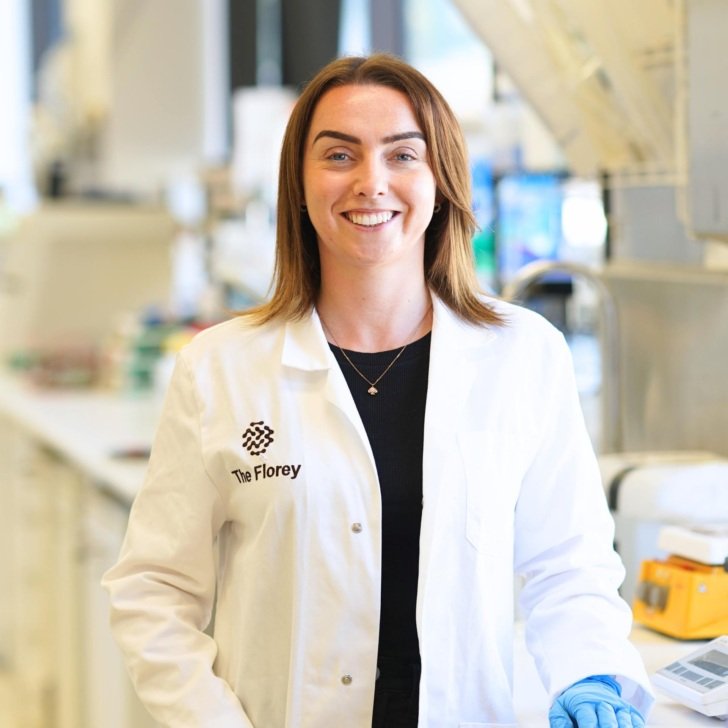
When we spoke, Trevor was just completing two years as Director of the Florey Institute of Neuroscience and Mental Health, a world-class centre for brain research (others in Australia include Neuroscience Research Australia, the Queensland Brain Institute at the University of Queensland and the Brain and Mind Centre at the University of Sydney).
The Florey, set up in Melbourne in the 1970s, is named after the Australian Nobel prizewinner Howard Florey who, with fellow scientist Ernst Chain, worked out how penicillin could be used as an antibiotic in 1939. (Alexander Fleming had discovered penicillin a decade earlier but hadn’t been able to pinpoint its active therapeutic ingredients.) By 1943, with Florey’s involvement, the Brits and the Americans were mass-producing enough penicillin for their armed forces. Before then, as we’ve explained before, if you got a bacterial infection, it was often a matter of “fingers crossed” you got through it, and many didn’t.
As a young PhD student, Trevor decided on a career in neurology, the study of the nervous system, including the brain, “because there was so much potential”. “To put it crudely,” he told me, “neurology was still in the dark ages, and it was clear that neurological problems were really uncharted waters – and yet, we could do so much more.” Brain-oriented research is, in many ways, the last frontier in medical research, he says. At The Florey, “we’ve organised ourselves to be relevant to the community, not an ivory tower. We see our role, primarily, is to try and solve wicked problems.”
Q: Trevor, what’s not well understood about the human brain?
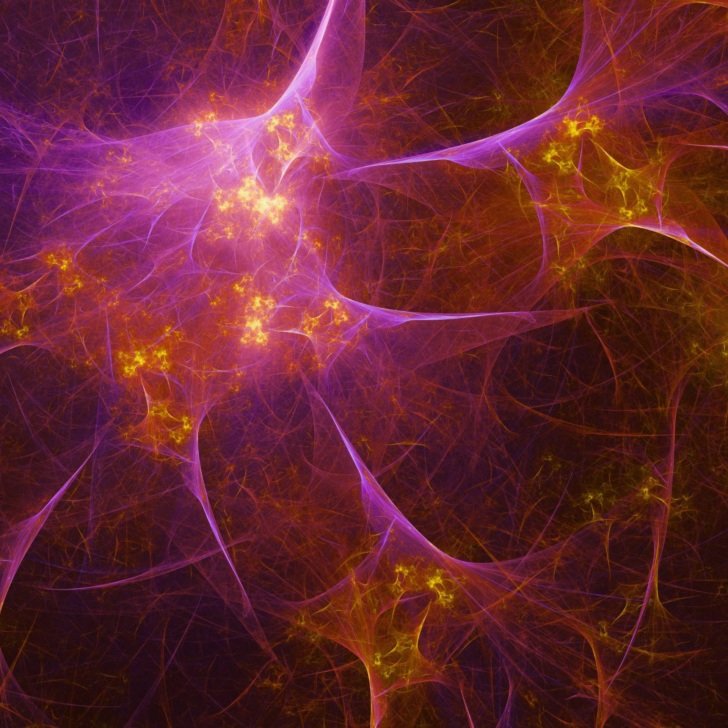
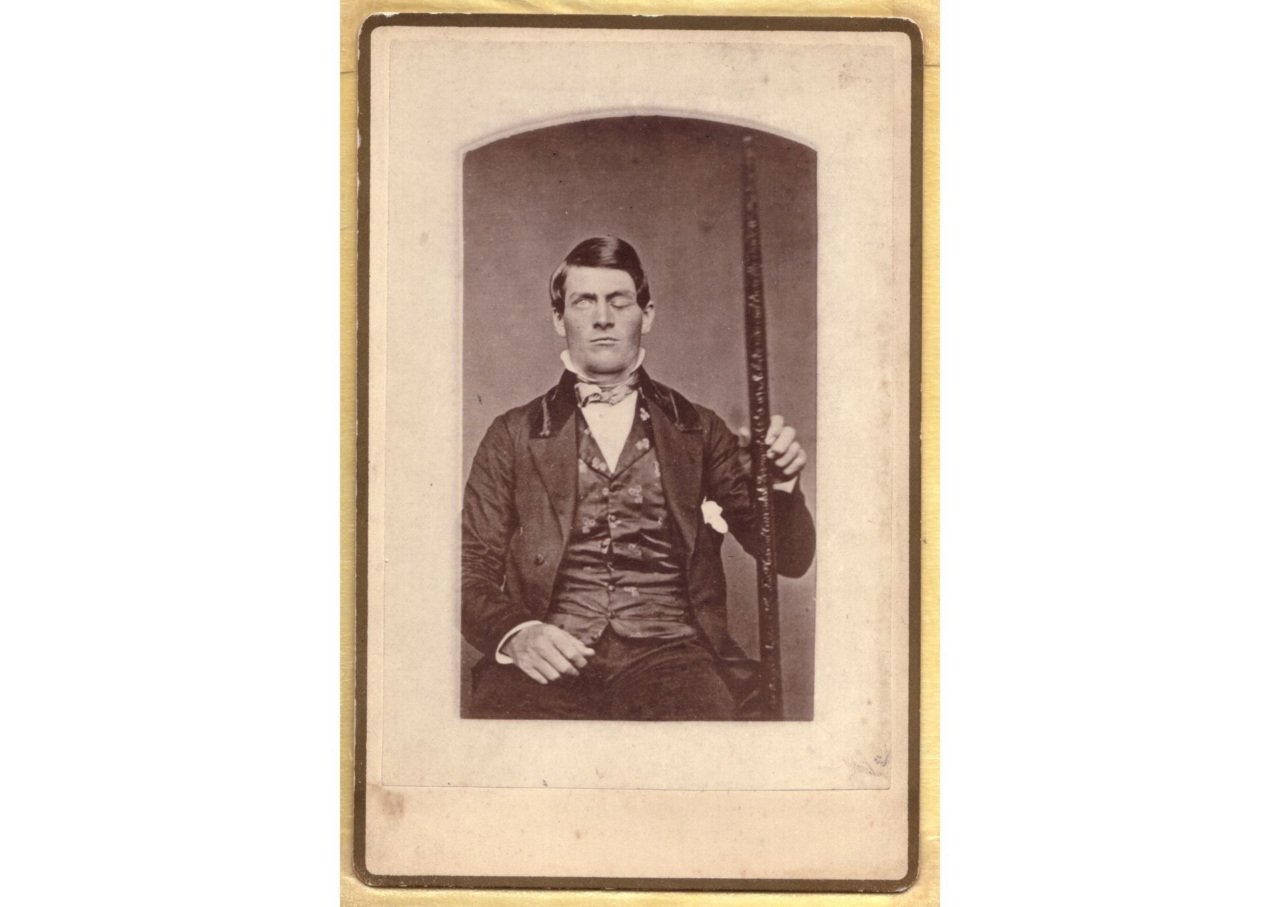
Well, first, the brain is not a computer. There was a famous case of Phineas Gage, an American railway worker who survived an unfortunate crowbar accident – the crowbar went right through the base of his skull – and a particular area of his brain was affected, but he was still able to function well, albeit with a change in personality. Gage’s case led to the perspective that there are discrete areas of the brain which do certain things. An investigator named Pierre Broca, a French physician in the late 1800s, really brought that to bear. But we now know the brain is much more sophisticated than that. Although those regions do exist, there are neural networks too. We need to understand better how they interact. It’s incredibly complex.
Q: What else is not understood about the brain?
There’s the old chestnut: what is consciousness? That’s a deep, fundamental question. We’re starting to understand that being awake and being asleep are very interesting complementary states that have developed during evolution. Sleep is important. It helps us lay down memories. We think it might be part of the process of working out how to predict circumstances based on our past experience – perhaps a key to how consciousness emerges. Sleep is also part and parcel of cleansing, of removing the garbage that accumulates in the brain during the day.
The other thing that’s misunderstood, for me, is about diseases of the brain. Abnormalities don’t emerge from nowhere. I think the idea that in your eighties you can protect against certain things is probably misplaced. Once you’ve got impaired memory, no number of crosswords or mental arithmetic is going to fundamentally change what happens to you in terms of the evolution of dementia. The key will be in pre-symptomatic diagnostics and preventatives 20 years earlier.
Q: So, what are the wicked problems you’re looking to solve?
Firstly, dementia. It’s become the most common cause of mortality, unfortunately, in women – the second-most overall. With the ageing population, this is becoming a tremendous problem: 400,000 people in Australia have dementia. It’s a tsunami. Alzheimer’s disease, the most common cause of dementia, is associated with a build-up of a deposit called amyloid. We know amyloid is deposited into the brain up to 20 years or so before symptomatic dementia develops. There has been recent development of disease-modifying drugs that, although imperfect and not yet approved by the Australian Therapeutic Goods Administration, are potentially game-changers – they remove the amyloid. We want to help with the rollout of those medicines, which will fuel a virtuous cycle of improved clinical care and research.
Q: This is what you meant just before when you spoke of garbage accumulating in the brain?
Spot on.
Q: What’s the second problem?
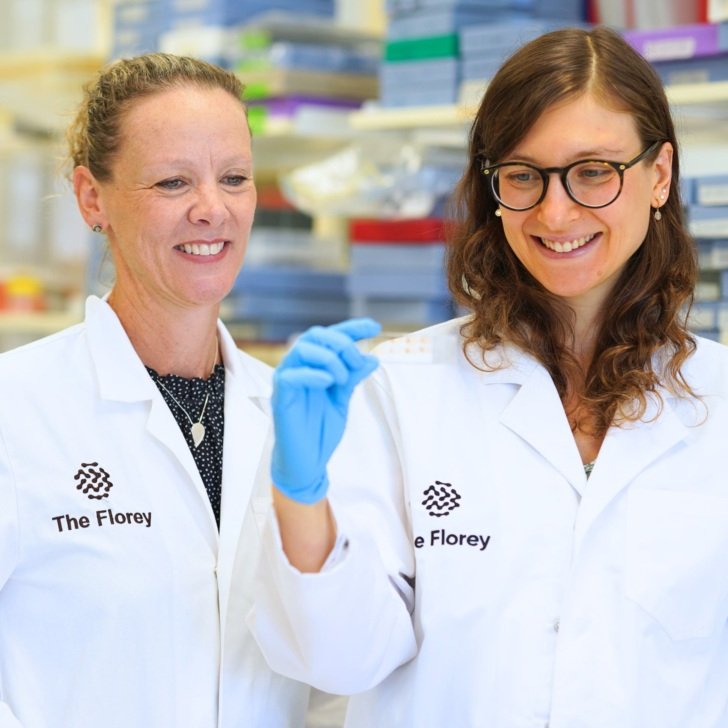
Epilepsy. At The Florey, we’ve got what we call the Australian Epilepsy Project, which is a $30-million medical research future fund project. We hope to give a much better quality of life to the third of people who are resistant to drugs for epilepsy. We’re also doing research into really bad forms of epilepsy, which can affect children in particular, to develop gene therapy. We’re on the cusp of a new world in being able to modify the lives of these kids.
Q: And alcoholism is on your radar?
Yes, we’re focusing on drug addiction, including to alcohol, and why some people are prone to it. We’ve found gender-related differences in how the brain is wired that influence people’s susceptibility. So there may be the need for sex-based treatments. That’s an important insight for the future.
Q: And schizophrenia?
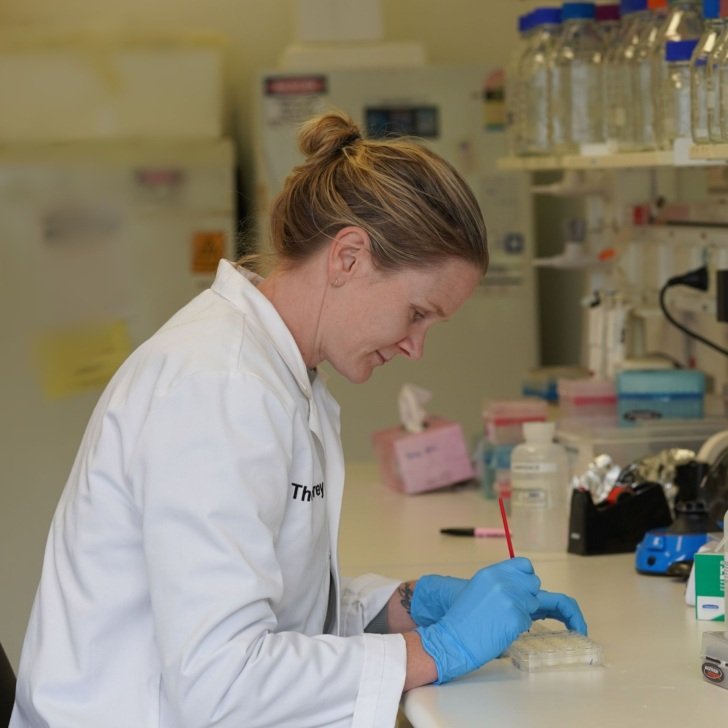
We’ve got a brain bank at The Florey. People who had mental health disorders, including schizophrenia, have generously donated their brains, and that has been very useful in understanding some of the molecular pathogenesis of schizophrenia. The US Food and Drug Administration is on the threshold of approving new therapy, a drug called KarXT, which really is, potentially, a game-changer.
Q: Your final focus?
Brain repair. This comes under the umbrella of “regenerative neuroscience”. We’ve taken cells from people unfortunate enough to have motor neurone disease (MND) and grown them into motor neurons. From there, we can assess the life history of those motor neurons. From that, we can identify drugs already licensed for treating other diseases which might have benefits for people with MND. Rather than having 150 clinical trials on 150 drugs, you can target it to one or two that show the most promise.
Q: And this can be applied to other conditions?
Yes, not least MS and Parkinson’s disease. Researchers are looking at transplanting neurons derived from stem cells to potentially treat Parkinson’s. A lot of the neurons lost in Parkinson’s disease are in one particular area of the brain, and it’s logical to think you might be able to replenish them. And a further approach is to develop organoids in a petri dish – mini-brains – to study their cellular dynamics in ways that we otherwise can’t do because we tend not to do brain biopsies, for obvious reasons.
Q: Indeed. Hang on, you’re growing mini-brains!
Pinhead size.
Q: So Trevor, what will you, personally, be working on now?
A lot of my attention will be on a particular type of receptor in the brain – they’re things that drugs bind to – which modulate the immune system and keep it finely tuned. They’re really important, not only in stopping pathogenic immune cells from getting out of control but also in removing debris in the brain, if you’ve got garbage like amyloid in Alzheimer’s or what’s called “myelin debris” in MS. Our focus is to help these receptors to do good things: either to nip the immune pathogenesis in the bud or, if there’s already progressive disease, to help them repair the damage.
This article was published as an Age and SMH Explainer newsletter.