- Inflammation occurs when our immune system responds to infection.
- Some neurodegenerative conditions like Parkinson’s, motor neurone disease, and Alzheimer’s are connected to inflammation.
- If we can regulate the immune system, we may also be able to find new treatments for diseases.
Inflammation: A delicate balance
When many of us use the word inflammation, we might apply it to describe the soreness we’re feeling in our back, our throat, or perhaps we’re told we have an ‘inflamed’ appendix.
But when researchers talk about inflammation, we’re referring to part of our body’s immune response. Inflammation is an underlying component in many of the serious neurodegenerative conditions we study at The Florey.
Ironically, although it can be damaging to our health, inflammation only occurs in healthy people whose immune systems are working properly and whose bodies can mount an appropriate response to infection.
When our immune system starts fighting infection, it initiates inflammatory responses that may cause acute symptoms in our tissues such as swelling, pain or flushed skin.
Ideally, once the immune system wins its fight against infection, tissues return to normal thanks to a variety of different kinds of immune cells that regulate inflammation like a ‘seesaw’.
These immune cells ensure adequate defence against attack by pathogens while preventing excessive inflammation – achieving a delicate balance that is just right for our body’s needs.
However, if our immune response ‘seesaw’ is not balanced, we may suffer lasting tissue damage and other debilitating chronic health conditions like insomnia, joint pain and fatigue.
Many neurodegenerative conditions also come hand in hand with inflammation, including Parkinson’s disease, motor neurone disease, and Alzheimer’s disease.
Given the close relationship between inflammation and the immune system, it’s clear that if we can regulate the immune system, we may also be able to develop new treatments for managing inflammatory diseases.
Indeed, the fields of oncology and autoimmunity have already made remarkable advances through immunotherapies, highlighting their potential in combating these conditions effectively.
Does inflammation affect the brain?
We’re learning about a close connection between inflammation and neurodegenerative conditions such as Alzheimer’s disease, Parkinson’s disease and motor neurone disease.
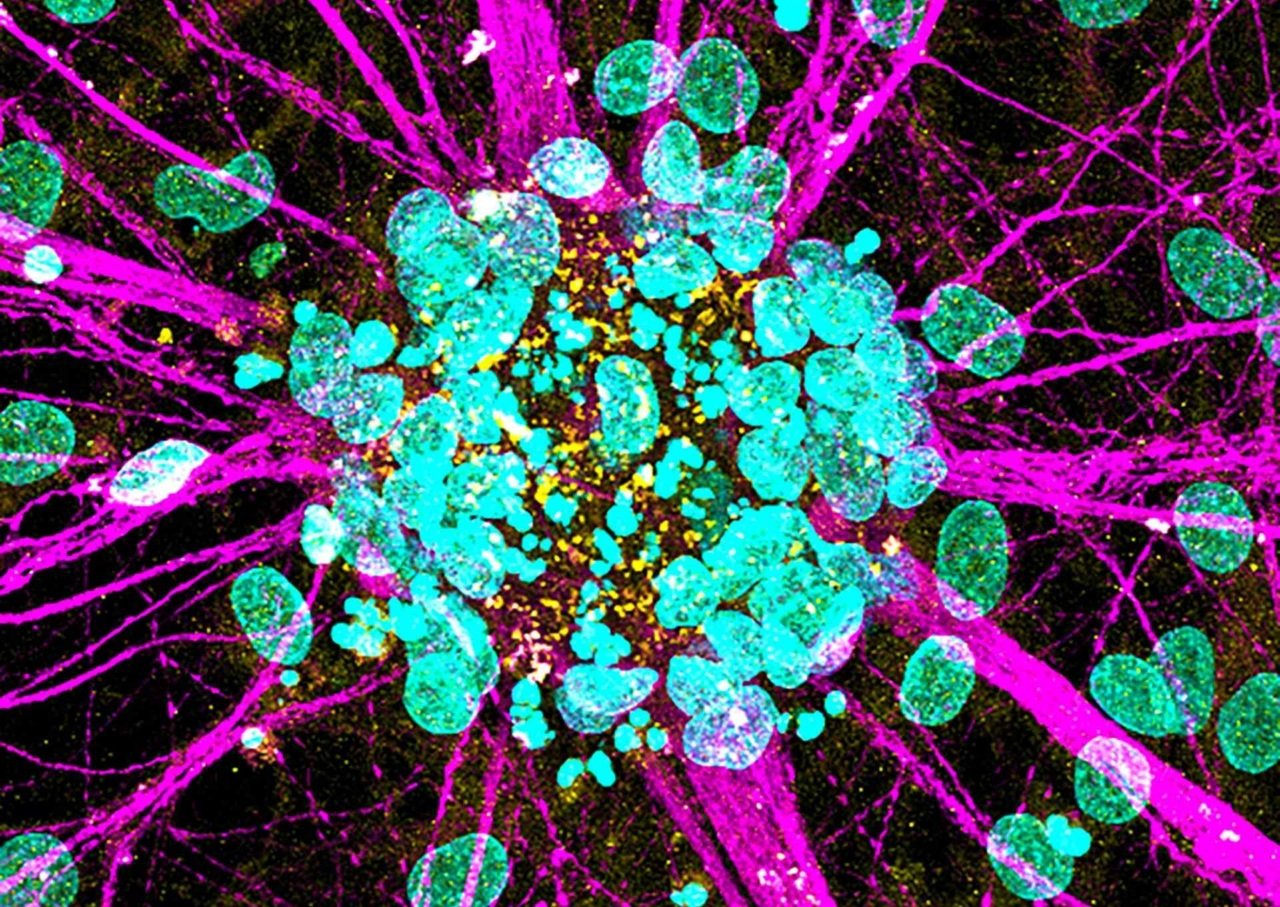
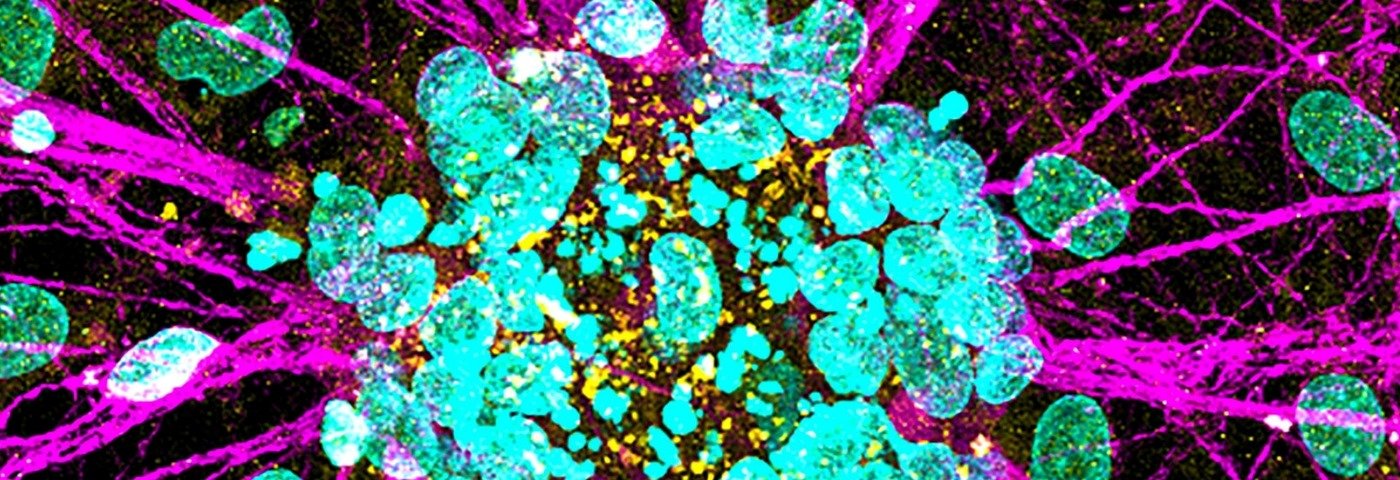
These conditions all cause an abnormal accumulation of proteins that trigger inflammatory responses, compromising cellular resilience and damaging molecules in the central nervous system, and speeding up the disease’s progress.
Scientists and doctors are trying to uncover what triggers these detrimental processes. Our aim is to find new ways to diagnose disease and intervene early enough to stop it developing.
Unlike inflammation elsewhere in the body, neuroinflammation is often subtle, complex and challenging to detect.
While recent clinical trials of immunomodulating agents have shown promise treating cancer and autoimmune diseases, there are still factors to consider when assessing their suitability as treatments for neurodegenerative diseases.
Firstly, until we understand the origins and underlying causes of these diseases, we’re limited to preventing onset and progression, which occur after the patient shows symptoms – rather than stopping people from getting the disease in the first place.
Secondly, many existing immunotherapies were originally developed to target the body’s tissues and cells and can’t penetrate the blood-brain barrier.
What can we do to treat neuroinflammation?
Our team and other researchers have recently discovered new ways to potentially target inflammatory pathways in the brain or spinal cord affected by motor neurone disease and some forms of dementia.
Unfortunately, current diagnostic tests only tell us when neurons have already died – they can’t tell us what disease the person has, and they can’t pick up cases before neuron death.
We’re working to develop new diagnostic methods to enable early detection and treatment of neurodegeneration at its earliest stages – before neurons die.
The pursuit of effective cures and treatments remains challenging for diseases that are multifaceted, with unknown causes and numerous triggers.

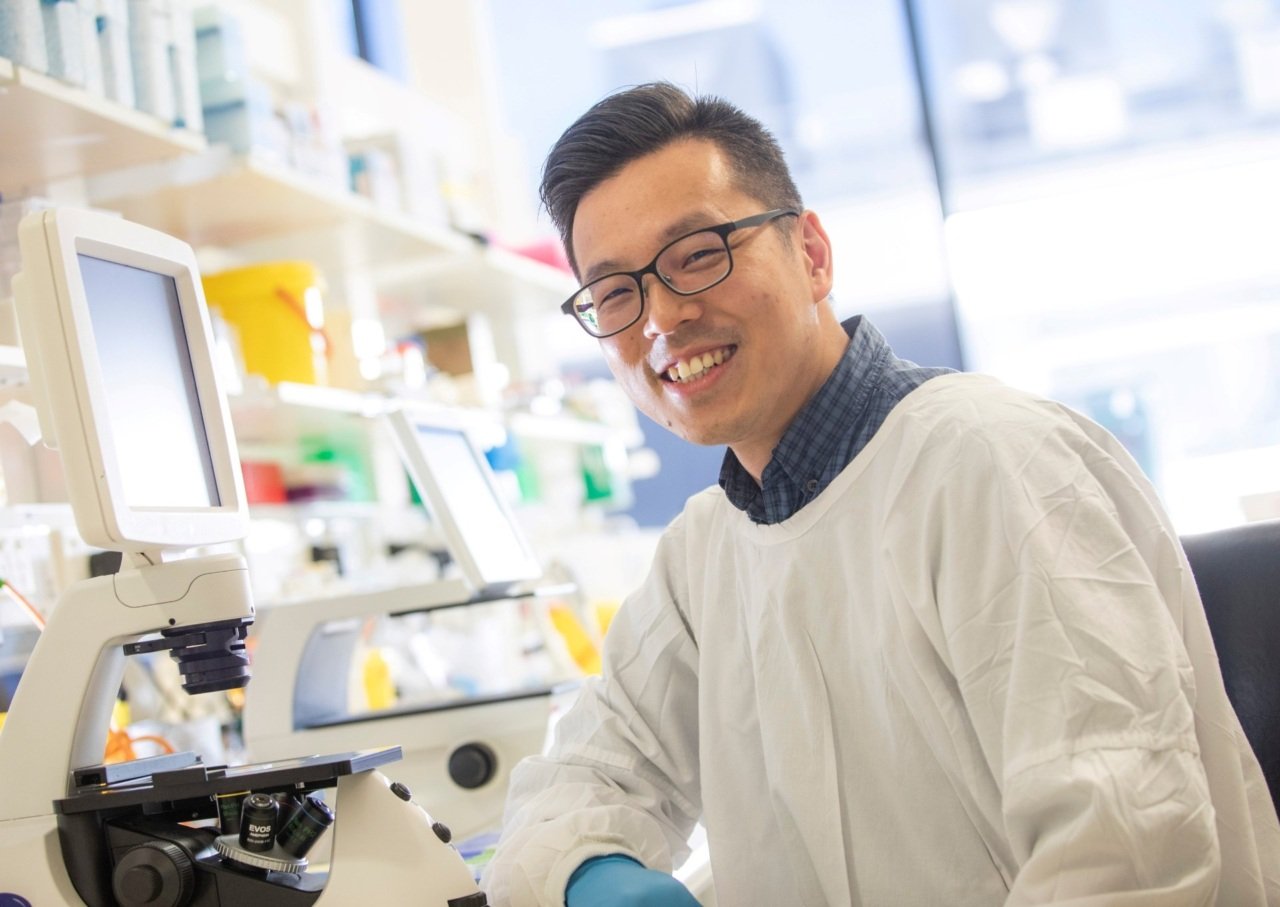
Supporting innovative ideas and fostering the careers of early- and mid-career researchers (EMCR) will significantly accelerate the search for a cure.
However, the establishment of interdisciplinary research programs has been increasingly crucial, uniting biomedical and clinical scientists, industry partners, patients, families, and caregivers.
Leveraging this collective expertise promises new discoveries, deepens our understanding of these conditions, and paves the way for innovative treatments and technologies.