- A genetic mutation in a sodium ion channel causes developmental and epileptic encephalopathy (DEE), a severe form of epilepsy that affects infants.
- For the first time, Florey researchers understand how the mutation prevents the brain from stopping seizure-inducing signals.
- The findings could have implications for current and future treatments of DEE.
The SCN2A gene and sodium ion flow
Florey researchers have discovered how a rare genetic mutation breaks a molecular ‘gate’, causing the severely disabling developmental and epileptic encephalopathy (DEE) in infants.
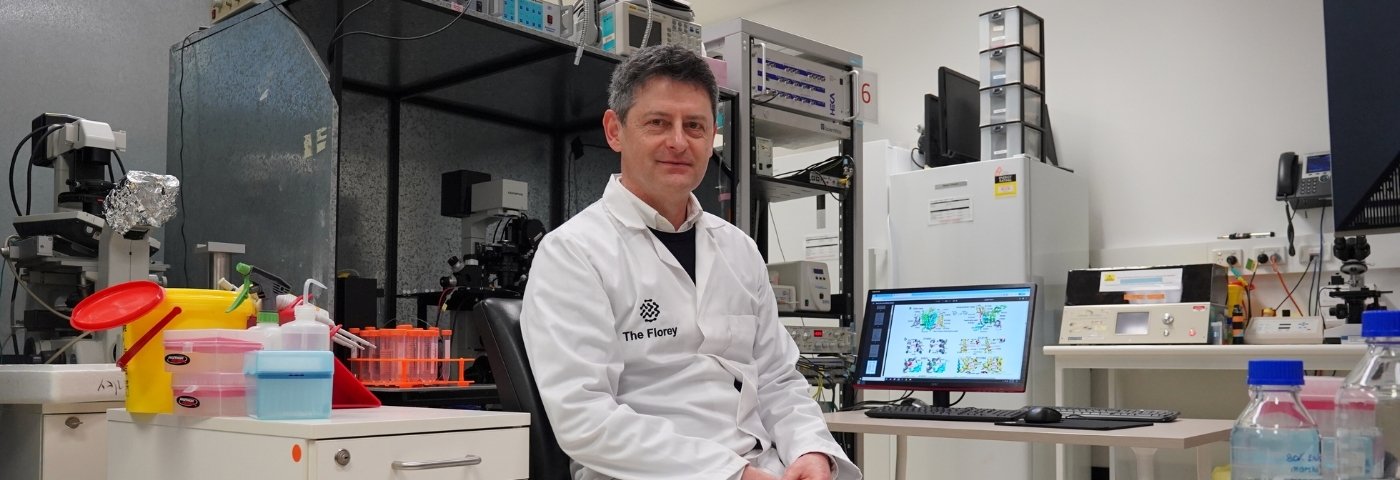
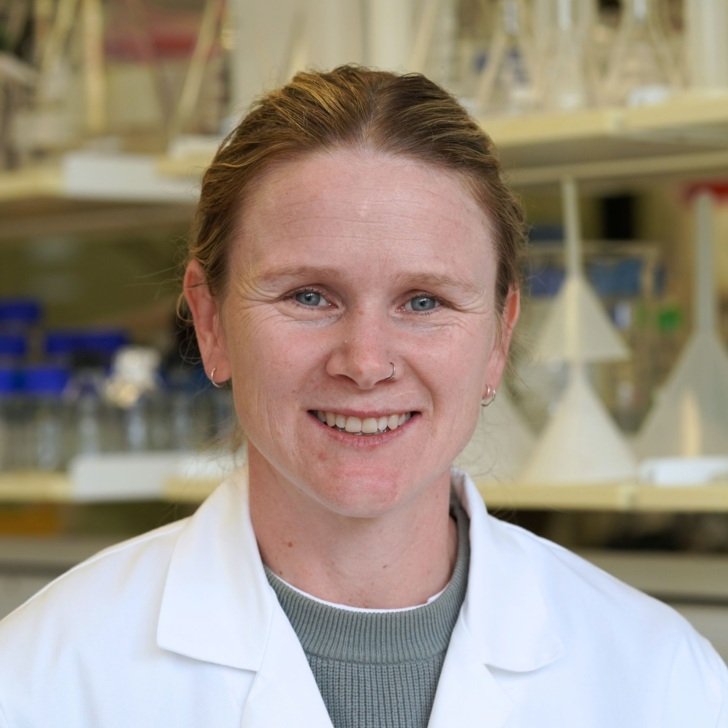
Florey biophysicist Dr Géza Berecki said DEE was a devastating condition that can start soon after birth, leading to severe disability or death.
Sodium channels are large proteins located in the membranes of neurons that possess a mechanism that works a bit like a self-closing gate.
“In healthy individuals, this cellular gate briefly opens then shuts automatically to prevent sodium ions from continuously flowing into neurons. We have discovered that in certain forms of DEEs – caused by mutations in the gene encoding the neuronal sodium Nav1.2 – the gate is always open, allowing the ions to flow continuously, leading to seizures,” Dr Berecki said.
The significant discovery is outlined in a paper published in Brain.

Dr Berecki, the paper’s first author, said precisely-timed sodium ion flow into neurons is part of normal brain signalling, but this is the first time researchers have shown that SCN2A mutations can cause uninterrupted sodium ion flow into neurons, leading to seizures.
“We worked with data of DEE patients in Australia and overseas, conducting experiments to measure neuronal function in cell samples and computer simulations of the mutation-affected protein,” said Dr. Berecki, from The Florey’s Ion Channels and Human Diseases Group.
“We found that the mutation in SCN2A that causes DEE disrupts fast inactivation of the Nav1.2 channel. This disrupts the brain’s ability to shut down neuronal signals, causing an overall increase in brain excitability.”
SCN2A is a very large gene which means it has immense potential for genetic variation. The number of distinct SCN2A mutations continues to grow as gene sequencing becomes more widespread.
Dr Berecki said that The Florey’s extensive research into genetic epilepsies, including SCN2A, not only deepens our understanding of ion channel diseases but also uncovers crucial new molecular interactions essential for the fast inactivation process in Nav1.2 channels.
“While these insights are significant for advancing fundamental science, they also hold promising therapeutic implications. Drugs capable of modifying the Nav1.2 inactivation mechanism may pave the way for more effective personalised treatment strategies for affected individuals,” Dr Berecki said.