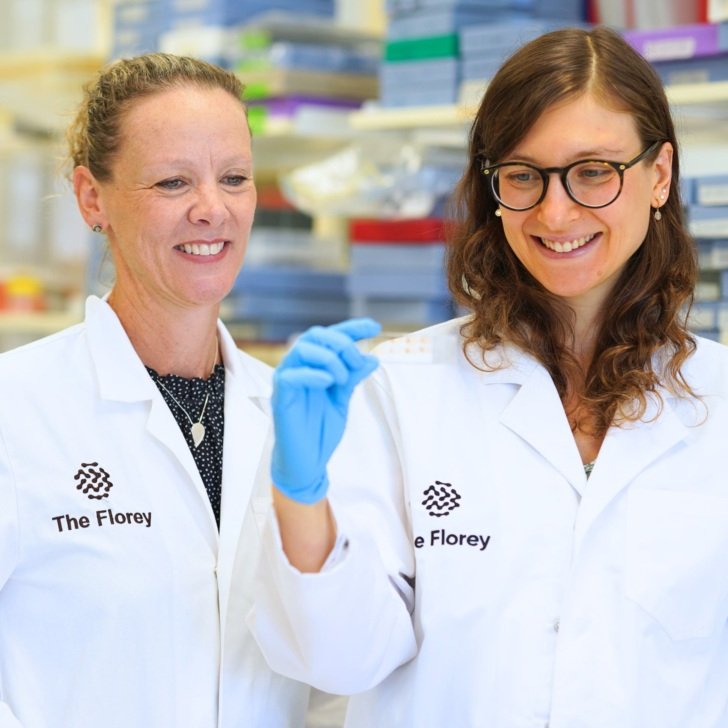
Researchers from the Australian Epilepsy Project (AEP) at The Florey are calling for changes to the way epilepsy is managed after a preliminary study highlighted differences in quality of life.
The early findings show that, from the initial 172 people studied:
- 64.5 percent were in paid work, but that dropped to 52 percent in people with drug resistant epilepsy.
- There was a lower quality of life than in the general population.
- Those not in paid employment had worse quality of life compared to those in paid employment.
- Almost 5.8 percent required formal care for on average of 20 hours per week.
- 17.7 percent required informal care of 16 hours per week on average.
- People with drug-resistant epilepsy had lower quality of life scores and were less likely to have paid employment compared to those newly diagnosed with epilepsy.
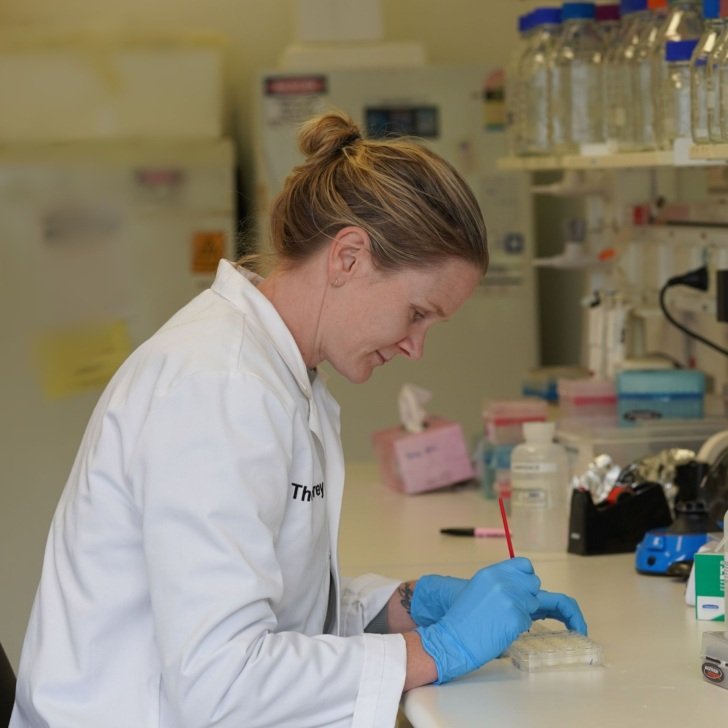
The pilot study of 172 people with epilepsy aged 18–65, sets the scene for a larger study underway at The Florey, as part of the AEP.

The project’s Health Economics Lead, Professor Zanfina Ademi, of Monash University, said the study published in Epilepsia Open supported international findings that epilepsy itself is not necessarily a barrier to paid employment, but other social economic variables come into play.
About 46 million people worldwide live with epilepsy, often with profound impact on their lives. Here in Australia, a radical shift is needed. This goes well beyond what can be achieved through changing an individual clinician’s practice or updating institutional policy.
Professor Ademi said: “An overhaul in the way epilepsy diagnostic and therapeutic care is delivered is a mammoth task but is likely the only effective way to dismantle existing barriers. We need more holistic management.
She said seizure control, adequate treatment of mood disorders, and accessible education are key factors for improving quality of life and employment prospects for people with epilepsy.
“Our research highlights the current quality of life for individuals affected by epilepsy, underscoring the urgent need for improvement. The Australian Epilepsy Project is spearheading an innovative approach to care, focusing on expediting diagnoses, enhancing the precision of detection, and improving patient outcomes, particularly for those who could gain from surgical procedures. This initiative is expected to lead to a reduction in the frequency of seizures or death, significantly improving the quality of life for those living with epilepsy,” she said.
Professor Ademi also called for better recognition of the role of carers.
“The often-overlooked contribution of caregivers to our economy is immense and should be a fundamental consideration in health economic analyses.”
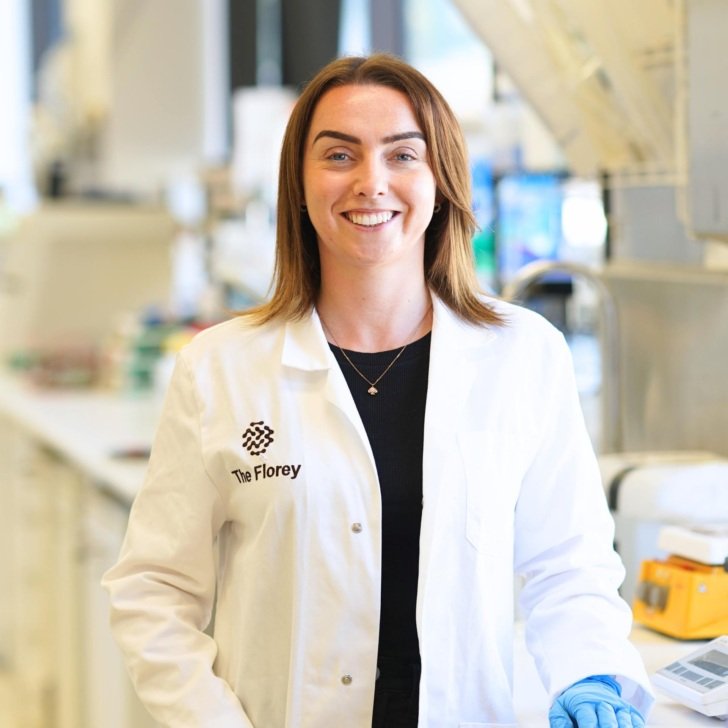
The AEP is founded and led by Chief Investigator, Florey Professor Graeme Jackson, and “represents a once-in-a-lifetime opportunity for Australian researchers and clinicians to effectively rewrite the books for epilepsy diagnosis and change lives”.