A multi-disciplinary team of experts and stroke survivors has rewritten the design rulebook for stroke rehab facilities.
The Neuroscience Optimised Virtual Environments Living Lab (NOVELL) project set out to inspire healthcare providers and designers to create innovative stroke rehab spaces that better support patient autonomy, activity and rest as part of their recovery journey.
Approximately 10,000 people with stroke were admitted for inpatient rehabilitation across Australia in 2020 (Stroke Foundation), and the average length of stay is 14 days*.
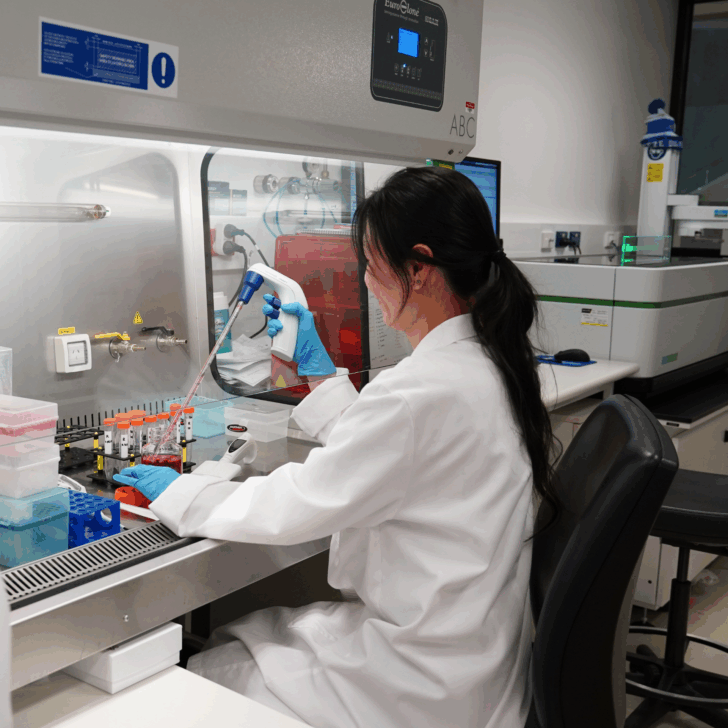
Using virtual reality technology and a collaborative, ‘living lab’ approach that incorporates ideas from stroke survivors, clinicians, architects, neuroscientists and policy makers, the NOVELL project has resulted in designs for purpose-built bedrooms and wards catering to recovery of stroke survivors.

Foundation objectives were to build:
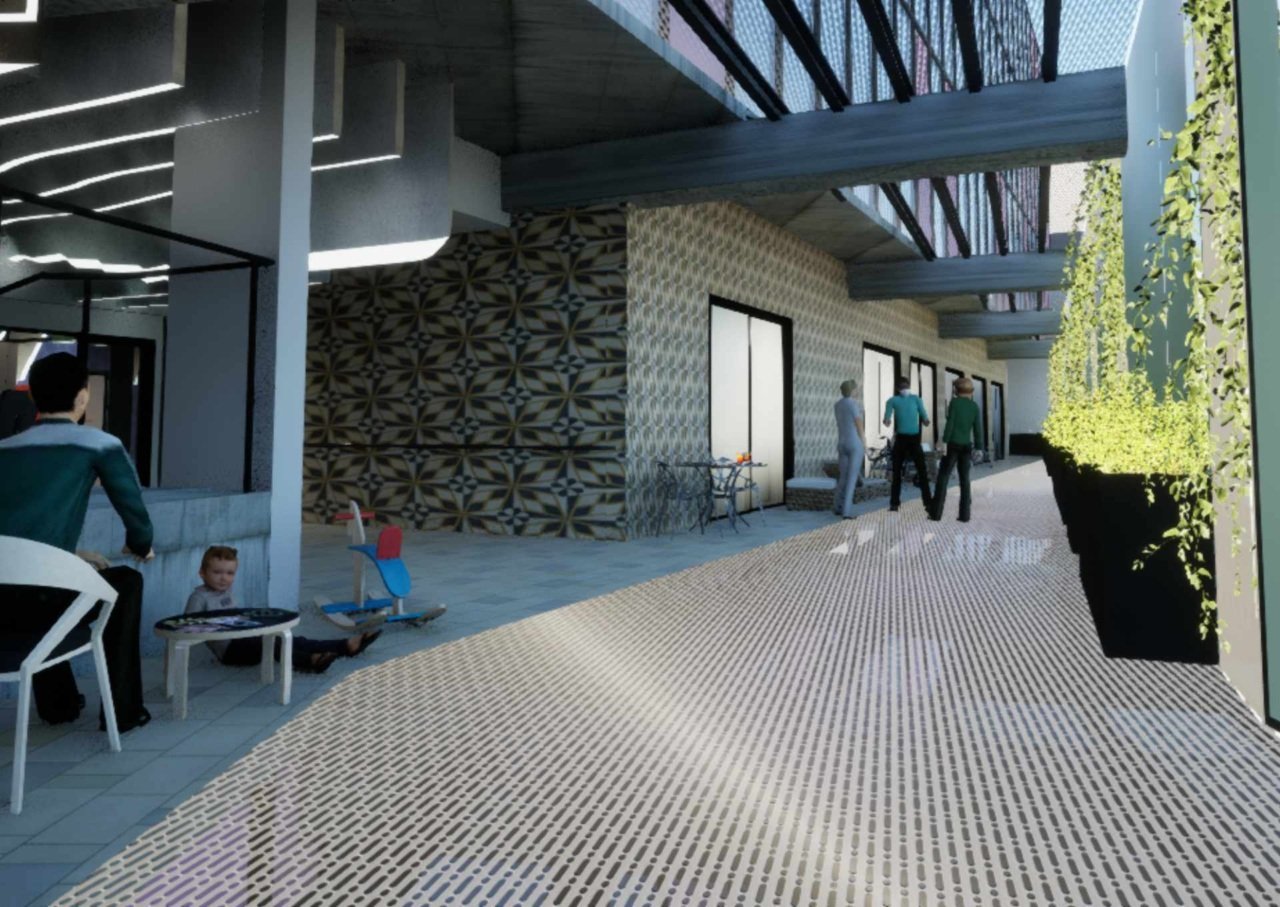
- A positive and stimulating environment, including communal spaces and other destinations to encourage people to get up and out of their bedrooms and keep active.
- Versatile spaces that can be adapted to meet different preferences and needs.
- Bedrooms that have all the benefits of both a single room (privacy, quiet for rest) and a shared bedroom (social interaction, safety).
- Better wayfinding to encourage confidence in leaving the room.
- Better lines of sight and visibility between stroke survivors and staff.
- Better access and visual connection to the outdoors.
Co-lead researcher Professor Julie Bernhardt from The Florey, said research suggests that people with potential to recover from stroke could do much better in the right environment, but about 70 per cent of rehabilitation facilities in Victoria are not purpose-built, and many more are designed following a model used for acute care.
Rather than encouraging stroke survivors to be active, many facilities subliminally encourage them to stay in their rooms, often in bed and alone. This is not helpful in promoting recovery after stroke.

“Our wards include carefully designed shared bedrooms where stroke survivors would have access to essential privacy and quiet time for rest, while also having opportunity to be stimulated through incidental social interactions with fellow stroke survivors, visitors and staff. There’s also some evidence suggesting that people in shared rooms are less likely to fall.”
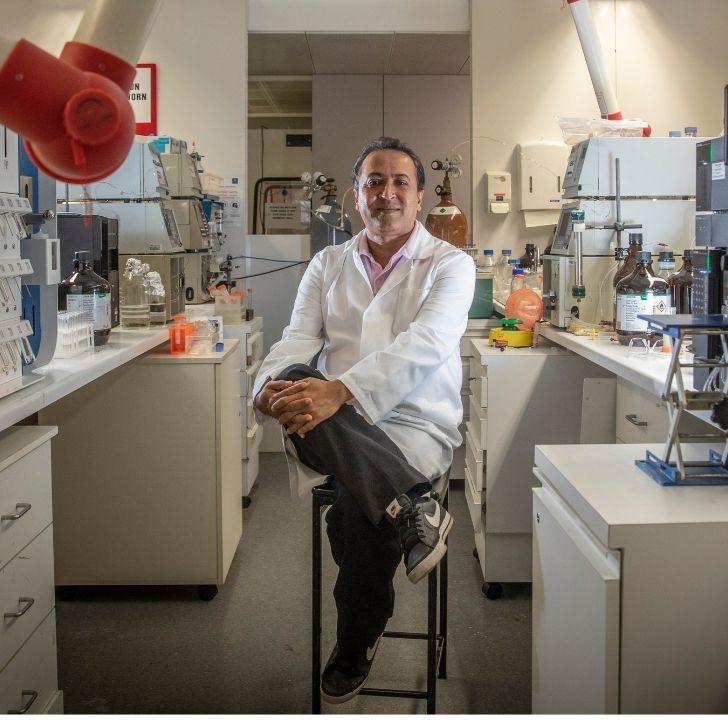
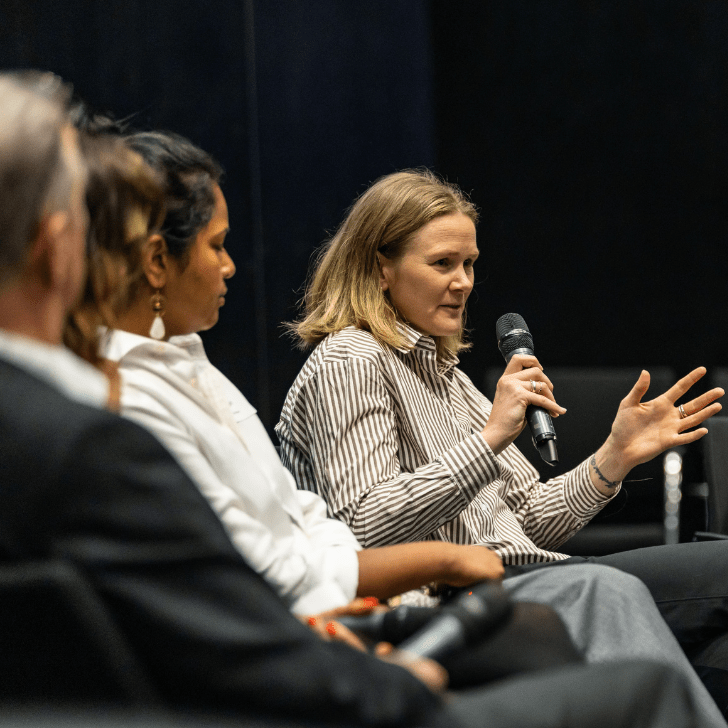
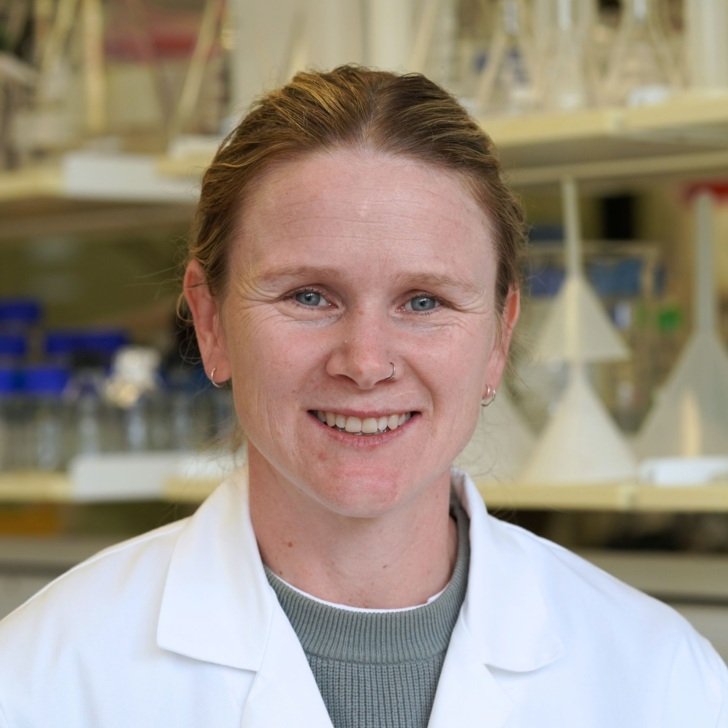
Professor Bernhardt said NOVELL brought together stroke survivors with experts from universities, healthcare workers, government, architecture, industry and the wider community to create and test a rigorous design process.
“We hope our ‘living lab’ framework will serve as a model design process in healthcare whether retrofitting existing spaces or building new facilities.”

Swinburne University of Technology Professor of Architecture and Urban Design, Professor Marcus White, who is co-leading the project, said rehabilitation facilities don’t have to be grim.
“These are spaces where people might be staying a few days, but could sometimes be there several months” Professor White said.
“A standard hospital design is just not fit for purpose. Careful design is needed that meets not only the purely functional aspects of the building, but also supports the physical and emotional wellbeing of those using it. We need to provide spaces that encourage connection between people as well as connection with nature.”

Professor White said the resulting designs synthesised a wide range of inputs from stroke survivors, clinicians, researchers, engineers and designers along with evidence from traditional academic literature, innovative performance modelling, and “built artifact evidence” through rigorous analysis of architectural precedents.
NOVELL’s results are expected to contribute to part of the next iteration of the subacute version of the Australasian Health Facility Design Guidelines which are currently under review.
* Australian Institute of Health and Welfare