Scientists from The Florey are among the world’s leading stroke experts who have mapped out how researchers and clinicians can improve outcomes for people who have survived a stroke.
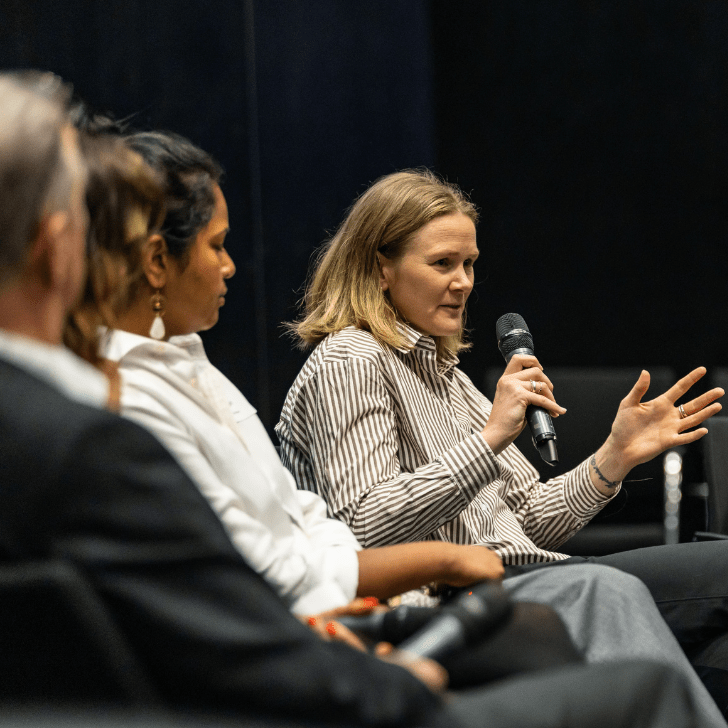
The third Stroke Recovery and Rehabilitation Roundtable, an initiative of the International Stroke Recovery and Rehabilitation Alliance, has made a series of key recommendations about managing fatigue, measuring mobility, harnessing non-invasive brain stimulation technologies and improving how trials are designed. The highly influential gathering of world stroke experts published their findings in a special edition of International Journal of Stroke.
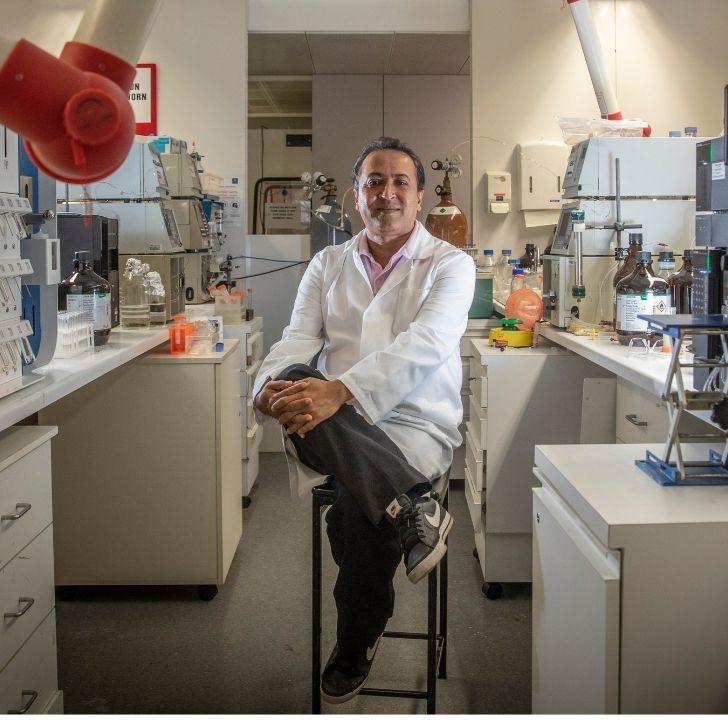
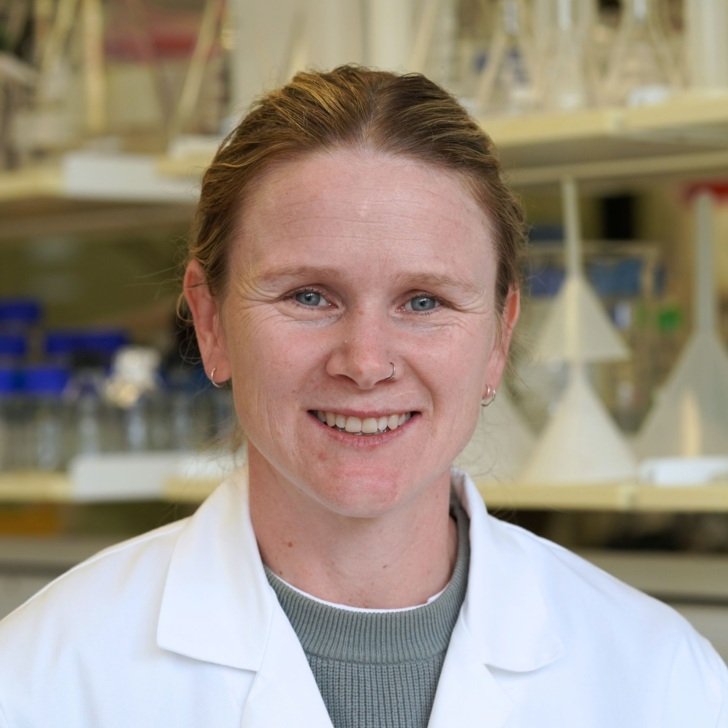
Associate Professor Kate Hayward from The Florey and University of Melbourne in Australia, co-chaired and convened the current roundtable, which was established by fellow Florey stroke expert Professor Julie Bernhardt in 2016.
“The roundtables aim to address gaps that are hampering progress across the field of stroke recovery and rehabilitation. Momentum is gathering in stroke recovery and it’s so important that we work together, pulling in the right direction, for the benefit of the millions of people globally who are affected by stroke,” Associate Professor Hayward said.
“Post-stroke fatigue, for instance, is common and complex, yet very little is known about it. To address this, an expert panel of researchers and people living with stroke sought to define fatigue, create a roadmap for future research and design a new fatigue assessment tool,” she said.
The Florey’s Professor Julie Bernhardt said the roundtable’s recommendations are essential reading for clinicians and researchers in the field of stroke recovery and rehabilitation.
It is through these collective actions that we can accelerate progress towards effective treatments that enhance the lives of the millions of people affected by stroke each year.
“The vision of our International Stroke Recovery and Rehabilitation Alliance is a world where global collaboration leads to major breakthroughs for people with stroke. Consensus building with these international taskforce recommendations is having impact and are an essential part of us achieving our vision,” Professor Bernhardt said.
Fatigue after stroke
The fatigue panel, led by University of Newcastle Professor Coralie English and University of Edinburgh Professor Gillian Mead, noted that fatigue affects almost half of all people living with stroke, yet there are no clear recommendations for preventing, recognising, treating or managing it.
The taskforce defined post-stroke fatigue as “a feeling of exhaustion, weariness or lack of energy that can be overwhelming, and which can involve physical, emotional, cognitive and perceptual contributors, which is not relieved by rest and affects a person’s daily life.”
They recommended that everyone who has had a stroke be assessed using a new Stroke Fatigue Clinical Assessment Tool, which asks a series of questions to ensure that fatigue isn’t missed, and to draw attention to potentially modifiable factors. Questions include whether the patient:
- feels tired all the time
- feels sad, depressed, anxious or stressed
- has trouble sleeping
- lacks exercise or misses meals
- has trouble remembering or concentrating
- feels fatigued after talking or listening to others talk.
The panel recommended future research investigates psycho-education interventions such as cognitive behavioural therapy, exercise, anti-depressants and neuromodulation therapies.
Fatigue taskforce co-lead, Professor English, said: “For many people living with stroke, fatigue is their number one issue. For too long this area of stroke recovery has been neglected in research. We hope our paper will inspire researchers to work in this area and motivate breakthroughs that will improve the lives of people living with post-stroke fatigue.”
Non-invasive brain stimulation and stroke
A second panel, led by University of Ottawa’s Associate Professor Jodi Edwards and University of Montreal’s Professor Numa Dancause, focused on finding ways to eliminate barriers for the use of non-invasive brain stimulation technologies as a treatment for stroke rehabilitation. The expert panel found that there is experimental and clinical evidence supporting such technologies as safe and potentially effective adjuncts to therapy post-stroke, yet their use is largely limited to treating major depression and pain.
Brain stimulation taskforce co-lead, Associate Professor Edwards, said: “Our panel sought to identify missing evidence for how to optimise these technologies for use as a standard treatment in post-stroke care. Surprisingly, we found that in addition to evidence gaps, there were major limitations with existing trials. This means as a field we are much farther from having the evidence necessary to optimize these technologies than initially thought. We propose a set of core recommendations and put forward a new checklist for future studies and clinical trials to help advance the field of brain stimulation post-stroke towards a pathway for translation to the clinic.”
Mobility and stroke
A third panel, led by Amsterdam University Medical Centre’s Professor Gert Kwakkel and KU Leuven’s Professor Geert Verheyden, recommended ways researchers can improve data on post-stroke mobility, a key priority for stroke survivors. The mobility panel said it was essential for researchers to use standardised instruments to enable data from different projects to be compared. The members also agreed on metrics, definitions and instruments that researchers should use to measure aspects of mobility including balance, walking independence and walking endurance.
Mobility taskforce co-lead, Professor Kwakkel, said: “Mobility problems are experienced by 80 per cent of stroke survivors and often the most important goal for many post-stroke as it affects their independence and quality of life. However, mobility is a complex construct that encompasses different domains that require different measurement instruments to assess recovery. In this panel, we achieved consensus on how and when to measure balance and mobility problems of people included in stroke recovery and rehabilitation studies.”
Research trials for stroke
The fourth roundtable, led by Associate Professor Hayward and Washington University Professor Catherine Lang, focused on trial design, specifically the control comparator group used in preclinical and clinical trials of stroke recovery interventions. This panel developed the CONtrol DeSIGN (CONSIGN) decision support tool to address challenges identified and enhance control comparator selection, description, and reporting.
Associate Professor Hayward, said: “Identifying an appropriate type of control to use in a preclinical or clinical trial is challenging, yet critically important. The benefit of an experimental intervention is established relative to a pre-specified control, and poor selection can reduce the ability to demonstrate a difference between the two.”