Currently there is no cure for the 400,000 people estimated to be living with MND globally, a disease characterised by muscle cramps, weakness and eventually paralysis in those who experience the condition.
A new paper from Dr Samantha Barton, Associate Professor Brad Turner and their team of MND researchers at the Florey investigates how a type of cell in the brain and spinal cord, known as oligodendrocytes, has the potential to contribute to the progressive loss of motor neurons in MND.
“Oligodendrocytes produce the protective coating on nerves in the brain and spinal cord, called myelin. The motor neurons that are lost in MND are coated in this insulating myelin sheath and it is essential for normal motor neuron health, function and survival. Despite its importance, its study remains relatively neglected in MND research,” said Dr Barton.
“We wanted to investigate the composition of the myelin sheath in MND patients to see to what extent oligodendrocytes are involved in the disease process. We can then determine if any changes occurring in the myelin sheath could be exacerbating motor neuron dysfunction and therefore contributing to their death,” continued Dr Barton.
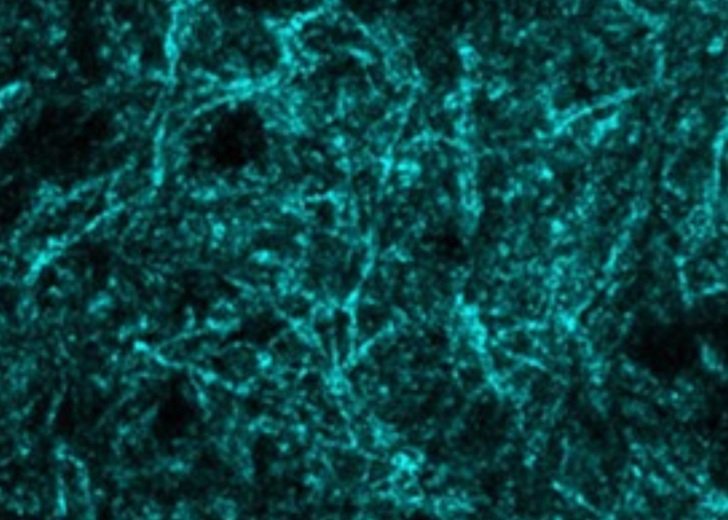
The team’s research compared MND patient post-mortem brain tissue samples to samples from people without MND, finding a significant difference in myelin composition between the two. A change to myelin composition would likely affect the normal functioning of motor neurons.
“By continuing to characterise how non-neuronal cells, like oligodendrocytes, and their disease pathways contribute to motor neuron dysfunction we hope to discover novel druggable targets for MND. These in turn open new pathways for potential treatments that target the whole disease,” said Associate Professor Turner.
“We will continue our study of oligodendrocyte involvement in MND using a combination of MND patient post-mortem tissue and MND patient stem cell models. We aim to determine whether preserving the health and function of myelin could improve motor neuron health and offer new hope to people living with MND,” said Dr Barton.
This research is now published in Metabolites: https://doi.org/10.3390/metabo12060554
This research was made possible by funding received from MND RA Jenny Simko MND Research grant, The Jane Frances Hayes and Frederick William Hayes Charitable Trust, Rebecca L. Cooper Medical Research Foundation Al and Val Rosenstrauss fellowship, Stafford Fox Medical Research Foundation, the Australian Government, and the Victorian Government.
