This ambitious 4-year program seeks to comprehensively map the genetic, molecular and biochemical makeup of patients using innovative stem cell models and systems biology approaches to predict and tailor treatment options for individual patients for the first time.
“I think the reason MND clinical trials have failed in the last 25 years is we group all patients together, so you can’t detect the benefit,” Dr Turner said.
“Once we get a disease signature we can start to address the treatment according to that profile, so every patient benefits, just like in cancer That’s the key difference.”
This program leverages biosamples from the largest MND patient stem cell resource in Australia collected at The Florey. Over 150 MND patient stem cell lines will be turned into motor neurons in culture and undergo deep profiling of genes, pathways and networks, aiming to generate a biological signature or ‘barcode’ for MND.
These biological barcodes will be correlated with clinical data and used to classify and subtype MND for the first time. The biological profiling of affected live motor neurons made accessible through stem cell technology in MND patients makes this program truly precision medicine.
The precision medicine program for MND will run in parallel with the FightMND drug screening program, allowing us to determine the right drug for the right patient. Ultimately, this program will lead to a better understanding of the Australian MND population and improved recruitment of patients into clinical trials.
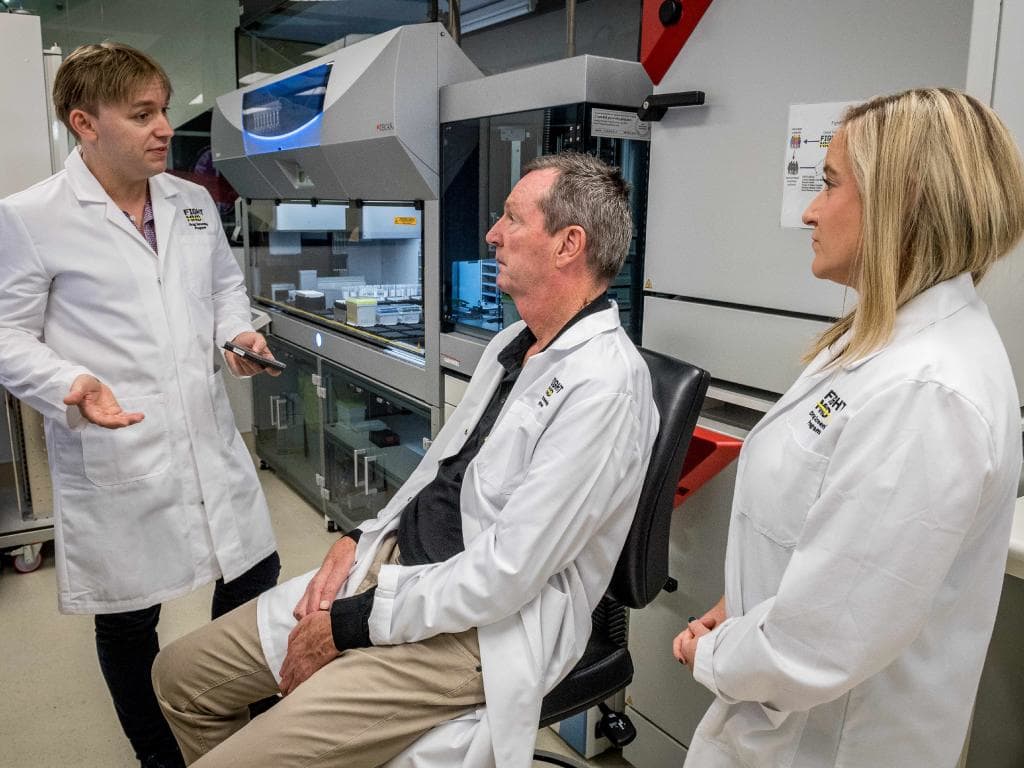
Neale Daniher, the AFL great and a founder of FightMND, was diagnosed with motor neurone disease almost six years ago when there were no promising treatments on the horizon.
“When there is no drug trial, there is no hope. But now there is hope,” he said.
The initiative is a large-scale national collaborative project which partners with MND patients and clinics, the Centre for Eye Research Australia, the Australian MND Registry and the Sporadic ALS Australian Systems Genomics Consortium.
